Where you live shouldn’t determine whether you can access colonoscopy services when you need them. However, new data shows there are stark differences in rates of MBS-subsidised colonoscopy across Australia, and that these gaps have grown over the last decade. How can we make sure some patients aren’t having colonoscopies unnecessarily while others with greater need miss out?
My conversations about colonoscopy with patients seem to be going one of two ways lately. On the one hand, I’m talking to people with no symptoms or risk factors for bowel cancer who are keen to have a colonoscopy due to recent media attention about bowel cancer. On the other hand, I have patients over 45 who need a lot of convincing to participate in regular bowel cancer screening with a faecal occult blood test.
These patient conversations highlight the mismatch between concern and clinical indication, and this is playing out on a larger scale than just my general practice. The reality is that the health system can struggle to meet the demand for colonoscopy services, and as with all healthcare resourcing, it is imperative that people are accessing colonoscopy for the right reasons at the right time.
If we zoom out to a national level, the interactive map of Australia in the latest Atlas of Healthcare Variation report (the Atlas) shows a clear pattern of higher rates of MBS-subsidised colonoscopy in major cities than in other areas. This is despite a higher rate of bowel cancer mortality outside major cities. If we look at the data by socioeconomic status, the most disadvantaged areas have the lowest rates of MBS-subsidised colonoscopy — so again the patterns of use and bowel cancer mortality don’t match.
Although we don’t know the ‘right’ rate of colonoscopy for a given area, looking at colonoscopies repeated within a short timeframe can give us further insights. The Guidelines for surveillance colonoscopy advise that only a small proportion of people (those at higher risk) need a repeat colonoscopy before three years. Unfortunately, Atlas data on MBS-subsidised repeat colonoscopy before the three-year mark again show discrepancies based on rurality and socioeconomic disadvantage.
A deepening divide
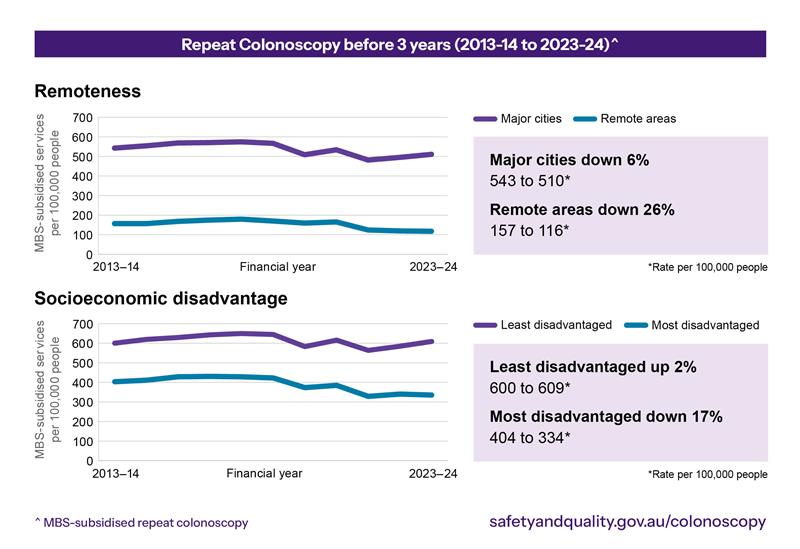
Trend data in the Atlas report shows that the variation has increased over the last decade. Nationally, the rate of MBS-subsidised repeat colonoscopy before three years fell by 8% between 2013–14 and 2023–24. However, the change over time has been very different for city dwellers than for people living in remote areas, and very different for those living in affluent areas compared to more socio-economically disadvantaged areas. Data for repeat colonoscopy before three years showed that over the last decade:
- major cities were down by 6%, remote areas were down by 26%; and
- the most disadvantaged areas were down by 17%, the least disadvantaged areas were up by 2%.
Again, these stark differences suggest not everybody has access to repeat colonoscopy when they need it, and some people are having it done too early, particularly in affluent areas.
Why are we seeing these patterns?
Some of the reasons for variation in rates of MBS-subsidised colonoscopy and repeat colonoscopy may be:
- availability of clinicians and health facilities;
- ability to pay, if there are out of pocket costs;
- awareness of bowel cancer symptoms and participation in screening;
- logistical barriers to access; or
- funding through models other than the MBS.
Increasing equity of access
Ensuring access to colonoscopy for everyone who needs it will need a sustained, multi-pronged approach. Many changes are already underway to help boost access to colonoscopy in the regions.
The Gastroenterological Society of Australia’s (GESA) Regional, Remote, and Indigenous (RRI) program has established Fellowship training positions in Darwin and Alice Springs, the Visiting Professor Program, and the Gut Centre Conference held annually in Alice Springs. These initiatives are driving sustainable workforce development while addressing health disparities experienced in regional and remote communities.
Other system level changes, such as financial incentives and outreach programs, are also needed to increase rates in underserved areas. GPs have an important role encouraging patients to take part in the National Bowel Cancer Screening Program, as only two in five eligible people currently participate.
While working to increase access in some areas, we also need to reduce inappropriate use of colonoscopy in others. Not only because we need to make better use of our finite healthcare resources, but because we should not be exposing patients to the risks of an unnecessary procedure, even if the risks are rare.
The revised Colonoscopy Clinical Care Standard (the Standard), released in September 2025 alongside the Atlas Focus Report: Colonoscopy, provides an updated national standard highlighting key aspects critical to quality colonoscopy. As a requirement for all health services delivering colonoscopy across Australia, the Standard mandates processes for referral, credentialling, the procedure, communication and follow up.
The Standard addresses two possible contributors to colonoscopies being repeated earlier than recommended: not being able to access a patient’s previous colonoscopy reports and not following surveillance guidelines. Colonoscopists should locate previous reports and confirm that a repeat colonoscopy aligns with the Clinical practice guidelines for surveillance colonoscopy before arranging it.
To mitigate this issue, the updated Standard guides health services and clinicians on best practice reporting and follow-up by uploading the colonoscopy report to both the patient’s healthcare record, as well as to shared record management systems such as My Health Record.
The Standard also has a stronger emphasis on the importance of communicating the colonoscopy report, histopathology findings and ongoing surveillance requirements to both the patient and their GP. Clear communication of the findings and the follow-up plan is key for avoiding performing repeat colonoscopy too early.
What’s happening in your area?
Healthcare services and clinicians can use the interactive data in the Atlas report to view colonoscopy and repeat colonoscopy rates in their local area to understand any gaps in care. Where there is variation, it is important to reflect on reasons for this and to act where needed.
Since 2018, the Colonoscopy Clinical Care Standard has supported the provision of high-quality colonoscopy for all Australians. The deepening divide in colonoscopy rates demonstrated in the new Atlas Focus Report: Colonoscopy shines a light on health inequity. To continue to build on Australia’s successes in detecting and treating bowel cancer, the healthcare system and clinicians need a united effort to ensure that all Australians, wherever they live, can access high-quality colonoscopy.
Dr Phoebe Holdenson Kimura is a Medical Advisor to the Australian Commission on Safety and Quality in Health Care and a general practitioner based in Sydney.
The authors do not work for, consult, own shares in or receive funding from any company or organisation that would benefit from this article, and have disclosed no relevant affiliations beyond their academic appointment.
The statements or opinions expressed in this article reflect the views of the authors and do not necessarily represent the official policy of the AMA, the MJA or InSight+ unless so stated.
Subscribe to the free InSight+ weekly newsletter here. It is available to all readers, not just registered medical practitioners.
If you would like to submit an article for consideration, send a Word version to mjainsight-editor@ampco.com.au.

 more_vert
more_vert
I didn’t enjoy my colonoscopies and would never have one as a screening test. But conversely I would pay $400,000 to have my life saved. Surely every medical procedure should have a good reason, but if people want to spend their money on herbal teas to lose weight rather than treatment supported by science, then they may indeed choose to pay for a colonoscopy without a good medical reason. If they are properly informed of the risks and if they are prepared to pay the full cost without shifting any of the cost to Government or to health funds then it is better they have a high quality colonoscopy in Australia than go overseas where they may get a low quality one. Perhaps a cheaper,safer test for CRC will come. Until then I suggest choose a good gastroenterologist and follow their advice.
The devil as always is in the detail. The key word in your data is MBS subsidized Colonoscopy. That means colonoscopies done in private facilities and billed to medicare. Those private facilities become fewer and fewer the more rural you go. Also as you pointed out the more rural you go the lower socioeconomic the status. So what we would expect is poorer people have less colonoscopies in private facilities, and MORE colonoscopies in public hospitals. Around 25% of colonoscopies in Australia are performed in public hospitals. The problem of access is not lack of facilities, as no one is going to build a colonoscopy facility in Marble Bar! The problem is distance and transport. Rural patients where I work are 40 minutes from a major public hospital, only those with no car have trouble getting there if they are physically unable to use the bus. But in more remote areas 3 hours from a public hospital transport is a problem for sick patients. Other types of incentives wont do anything.
The debate about inequality of access is completely overshadowed by the issue of whether colonoscopy should be used as a screening tool at all. It undoubtedly reduces mortality from bowel cancer but at what cost? About a million colonoscopies are performed every year in Australia at a cost of some 2 billion dollars. The vast majority are for screening. The incidence of CRC is about 15,000 new cases every year. Assuming a 30% reduction with screening (depending on which study you read) this equates to about 5000 lives saved at a cost of $400,000 each. A conversation gastroenterologists don’t want to have. And that doesn’t include the cost of the FOBT program, which is perfectly justifiable on its own. And it certainly doesn’t include the cost of litigation. As a colorectal surgeon I have performed thousands of colonoscopies over a 40 year period. I now perform none because I would have to abide by the guidelines (for the purposes of a ridiculous re-accreditation scheme) which I consider to be ludicrously over-prescriptive and it is frankly unconscionable. I do however have a huge medicolegal practice and will continue to write reports for lawyers handling a perforated a colon. This is a recognised risk of colonoscopy but when the procedure is done for no good reason, there’s a lot of fast talking to be done. It would also help to explain the unsustainable rise in indemnity insurance premiums. On a final note it would be good if the discussion could include the 1.5% of the health budget spent on prevention when it is well-proven that CRC (in addition to everything else) is significantly increased with obesity. I’ve published extensively about this just in case anyone wants to have a go.