Dementia represents one of the greatest public health challenges of our time. It encompasses a range of neurodegenerative disorders marked by progressive cognitive decline, memory loss and loss of independence. Among these diseases, Alzheimer’s disease (AD) is the most prevalent, accounting for approximately 60–70% of all dementia cases worldwide.
First described by Alois Alzheimer in 1906, Alzheimer’s disease is characterized by the accumulation of amyloid-beta plaques and neurofibrillary tau tangles in the brain. These pathological changes are associated with neuronal death and widespread brain atrophy, with tau pathology playing a key role in disease progression. In Australia, the impact of AD is intensifying. In 2025, the Australian Institute of Health and Welfare reported that dementia had become the leading cause of death, surpassing ischemic heart disease. This sobering reality underscores the urgent need for innovative diagnostic and therapeutic strategies, ones capable of identifying AD earlier, intervening more effectively and ultimately altering its trajectory.
The promise of nanoparticles in Alzheimer’s research
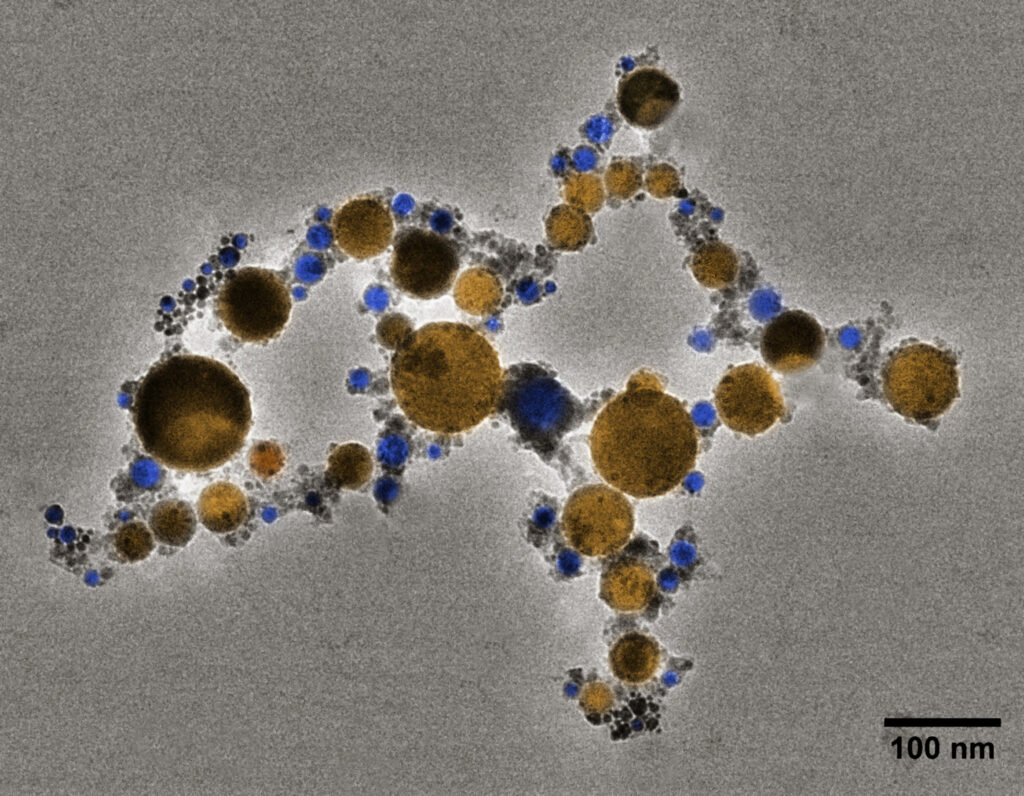
Nanoparticles, materials ranging between 1 and 100 nanometres, may hold the key to the next generation of Alzheimer’s diagnostics and treatments. Although nanoscale materials such as colloidal gold have been used for centuries, modern nanotechnology began to take shape in the 1980s and rapidly revolutionized biomedical science in the decades that followed. Thanks to their high surface area-to-volume ratio and modifiable chemistry, nanoparticles can be engineered to carry therapeutic drugs, targeting molecules and imaging agents simultaneously. This versatility enables them to function as “theranostic” platforms — delivering both diagnosis and treatment within a single system.
In Alzheimer’s disease research, their potential is compelling because they offer a unique advantage: they can be tailored to cross the blood-brain barrier (BBB) — a formidable obstacle in neurological medicine — and selectively bind to pathological targets such as amyloid-beta or tau. Once there, they can deliver therapeutic payloads precisely where they are needed. This capability represents a step toward true precision medicine in neurodegenerative disease: targeted, efficient and minimally invasive.
Bridging the gap: challenges in translational nanomedicine
Despite their immense promise, nanoparticle-based therapies face considerable barriers on the path to clinical translation. The first FDA-approved magnetic nanoparticles, introduced in the early 2000s as MRI contrast agents, demonstrated feasibility but limited visibility. Their signal-reducing nature made quantification difficult, curtailing their diagnostic impact.
To enhance imaging performance, researchers began attaching fluorescent dyes or radiolabels to nanoparticles, but these modifications introduced new problems, including unpredictably altered biodistribution, unpredictable pharmacokinetics and increased regulatory complexity. A key biological obstacle is the protein corona effect: when nanoparticles enter the bloodstream, plasma proteins rapidly absorb to their surface, changing their biological identity. This process can mask targeting molecules, shift the surface charge and accelerate clearance by the reticuloendothelial system (RES), notably the liver and spleen. Overcoming these barriers is critical to translating nanoparticle research from promising theory to clinical reality.
Magnetic particle imaging: a game-changer in neuroimaging
Magnetic particle imaging (MPI) is emerging as a breakthrough technology capable of overcoming many of the challenges. Introduced by Philips Research in Germany in 2005, MPI enables the direct, real-time detection of superparamagnetic iron oxide particles (SPIONs), with unparalleled sensitivity and zero background noise.
Unlike MRI, which relies on indirect contrast and suffers from low sensitivity to magnetic nanoparticles, MPI offers a linear and quantifiable signal that correlates directly with the nanoparticle concentration. This makes it ideal for tracking biodistribution, monitoring drug delivery, and mapping disease progression in conditions such as AD.
Beyond diagnostics, MPI’s integration with nanomedicine offers theranostic possibilities. For instance, curcumin, a natural anti-inflammatory and anti-amyloid compound, can be conjugated to magnetic nanoparticles. This dual-functional system allows researchers to visualize amyloid plaques while simultaneously delivering anti-inflammatory therapy — representing a paradigm shift in Alzheimer’s research, combining detection and treatment in one targeted intervention.
Another promising application is magnetic hyperthermia, where an external alternating magnetic field is applied to heat magnetic nanoparticles localized in a region of interest. Already under clinical investigation for cancer therapy, this technology could one day be applied in Alzheimer’s disease to disrupt toxic protein aggregates or enhance drug penetration across the blood-brain barrier. The ability to precisely control heat generation opens new avenues for noninvasive neuromodulation and localized therapy.
Australia’s opportunity to lead
Australia stands at a pivotal moment in this emerging field. With two preclinical MPI systems now operational nationally — including leading work at UNSW’s Centre for Healthy Brain Ageing (CHeBA) — our researchers are uniquely positioned to contribute to global advances in neuroimaging and nanotherapeutics.
This infrastructure enables Australian researchers to overcome longstanding quantification challenges with unprecedented accuracy, validate targeted delivery in vivo and accelerate the development of next-generation nanomedicines. As MPI technology evolves, potentially toward portable, bedside systems, its integration into dementia research could fundamentally transform how we detect, monitor and treat neurodegenerative disease.
In a world where dementia is fast becoming the defining health crisis of an ageing population, innovation is not optional — it is imperative. The convergence of nanotechnology and magnetic particle imaging represents more than a scientific milestone; it is a pathway to hope for millions of individuals and families touched by Alzheimer’s disease.
Dr Saeed Shanehsazzadeh is a Research Associate at CHeBA. He holds a PhD in Medical Physics from Tehran University of Medical Sciences and has over a decade of experience in molecular imaging, nanomedicine, and multidisciplinary medical sciences labs in Iran, Germany, Belgium, Canada, Singapore and Australia. His work focuses on advancing magnetic particle imaging (MPI) as a novel method for detecting early changes in the brain related to neurodegenerative diseases.
Professor Perminder Sachdev AM is a Scientia Professor of Neuropsychiatry and Co-Director of the Centre for Healthy Brain Ageing (CHeBA) in the Discipline of Psychiatry and Mental Health at the University of New South Wales (UNSW Sydney), with research and clinical interests including neuropsychiatric disorders of older people and disorders of cognition, vascular dementia, Alzheimer’s disease, dementia of Lewy Body type, and Mild Cognitive Impairment. He is also Clinical Director of the Neuropsychiatric Institute (NPI) at the Prince of Wales Hospital and Deputy Chair of the Australian Dementia Network (ADNeT).
The statements or opinions expressed in this article reflect the views of the authors and do not necessarily represent the official policy of the AMA, the MJA or InSight+ unless so stated.
Subscribe to the free InSight+ weekly newsletter here. It is available to all readers, not just registered medical practitioners.
If you would like to submit an article for consideration, send a Word version to mjainsight-editor@ampco.com.au.

 more_vert
more_vert