New research uncovers how socio-economic disparities influence antibiotic use in Australia, providing critical tools to address AMR.
Antimicrobial resistance, also known as AMR, poses a major global health threat, resulting in an estimated 5 million deaths in 2019, and projections indicating up to 10 million deaths annually by 2050. In Australia, hospitals spend more than $11 million per year treating just two AMR-related hazards — ceftriaxone-resistant Escherichia coli bloodstream infections and methicillin-resistant Staphylococcus aureus infections.
The misuse and overuse of antibiotics remain as primary drivers of AMR. While low income countries often experience significant antibiotic consumption due to rapid socio-economic changes, Australia’s per capita antibiotic use stands out among high income nations, contrary to the downward trends observed in other high income countries.
Australia’s antibiotic monitoring efforts have predominantly focused on hospital settings, where stewardship programs have been implemented. In contrast, community antibiotic use relies heavily on data from the Pharmaceutical Benefits Scheme (PBS). However, PBS data have notable limitations, such as the inability to capture all antibiotic use, the lack of real-time reporting, and insufficient reflection of the relationship between antibiotic use and population characteristics. These gaps hinder comprehensive understanding and effective public health responses to AMR.

Examining antibiotic use through wastewater data
While the widespread detection of antibiotics is not unexpected, our study uncovered a more nuanced story by assessing antibiotic consumption against socio-economic disparities. Communities with greater socio-economic advantages — characterised by higher income, better education, improved access to health care, and favourable living conditions — were found to use antibiotics more frequently and in larger quantities. These groups possibly benefit from easier access to medical services, face fewer financial barriers, and are generally more proactive in seeking medical care — all contributing to their higher antibiotic consumption. Conversely, communities with fewer socio-economic advantages exhibited relatively lower antibiotic use. Factors such as limited access to health care, financial challenges, and logistical barriers were likely to blame. These barriers can delay or prevent timely treatment, limiting the use of necessary medications.
These findings were achieved using wastewater analysis by our team at the University of Queensland. Wastewater samples were collected from 50 treatment plants across the country, representing half of the population on the 2021 Australian Census Day. We then analysed 102 compounds and cross-referenced results against census data to explore how socio-economic factors, such as income, education and housing density influence antibiotic use.
Antibiotic residues were commonly found in Australian wastewater, underscoring their widespread use and potential environmental impact. Among the 41 antibiotics and 15 related compounds detected, cephalexin and ciprofloxacin stood out as the most frequently used, appearing in every sample. These findings highlight the extensive use of these antibiotics in both health care and community settings. Amoxicillin, another widely prescribed antibiotic, was also found in significant amounts alongside its breakdown products.
The link between antibiotic use and socio-economic factors shows the pattern of unequal antibiotic use and reflects both the privileges and challenges faced by different socio-economic groups. For higher socio-economic status communities, easy access to medical resources can sometimes lead to overprescription and misuse, contributing to the global challenge of AMR. On the other hand, lower socio-economic status communities may face the opposite problem, where limited resources result in delayed or inadequate treatment, exacerbating health disparities.
Implications for public health policy
The findings call for tailored approaches to antibiotic stewardship. Addressing both the overuse of antibiotics in affluent communities and potential underuse in disadvantaged areas is critical to achieving equitable health care outcomes.
For high income communities, targeted education campaigns could raise awareness about the risks of antibiotic overuse and its contribution to AMR. These initiatives should emphasise the importance of adhering to medical guidelines and avoiding unnecessary prescriptions. Conversely, in low income areas, government interventions to improve health care accessibility and affordability are essential. Subsidised health care services and community health programs could ensure timely treatment for infections, reducing reliance on antibiotics as a first-line defence.
Urban planning and housing policies also play a pivotal role. Overcrowded living conditions exacerbate infection risks, which our data shows leads to higher antibiotic use.
Investing in public health infrastructure to address these conditions could mitigate the need for excessive antibiotic prescriptions.
Next steps in combating AMR
To strengthen Australia’s AMR response, integrating these findings into national and regional health strategies is vital. We previously demonstrated that wastewater surveillance not only allows us to identify the immediate impacts of interventions but also assess the long term effectiveness when we evaluated the introduction of a minimum unit price for alcohol in the Northern Territory. As such, our key recommendations include:
- Expanding wastewater surveillance: implementing long term wastewater monitoring programs to track both antibiotic consumption and AMR resistance genes to identify emerging trends.
- Enhancing education and outreach: developing targeted campaigns to educate both health care providers and the public about responsible antibiotic use.
- Improving health care equity: ensuring all Australians have access to timely and affordable medical care, particularly in under-served communities.
- Addressing environmental drivers: investing in urban health programs to improve living conditions and reduce infection risks in overcrowded areas.
- Strengthening policy frameworks: enforcing stricter regulations on antibiotic prescribing and promoting antimicrobial stewardship across all health care settings.
Australia’s comprehensive census data and availability of advanced analytical methods, combined with extensive experience in wastewater-based epidemiology provide a strong foundation for these initiatives. In addition, by leveraging and extending the National Wastewater Drug Monitoring Program (NWDMP) to include AMR and antimicrobial use, policy makers can design evidence-based interventions to combat AMR effectively.
Conclusion
The findings of this study underscore the critical role of socio-economic factors in shaping antibiotic use patterns. By addressing these disparities, Australia can lead global efforts against AMR. Policy makers, health care providers and public health officials must work collaboratively to implement the recommendations outlined, ensuring antibiotics remain a viable tool for future generations.
This research, supported by data published in Nature Water, demonstrates the value of integrating environmental and social data to inform public health strategies. For a detailed exploration of the study’s findings, visit Nature Water.
Mr Jinglong Li is a PhD student in environmental health science at the Queensland Alliance for Environmental Health Sciences (QAEHS), The University of Queensland.
Dr Jake O’Brien is an NHMRC Emerging Leadership Fellow in environmental health sciences at The University of Queensland’s research centre the Queensland Alliance for Environmental Health Sciences.
Professor Kevin Thomas is an environmental health scientist and Director of The University of Queensland’s research centre Queensland Alliance for Environmental Health Sciences.
The authors do not work for, consult, own shares in or receive funding from any company or organisation that would benefit from this article, and have disclosed no relevant affiliations beyond their academic appointment.
The statements or opinions expressed in this article reflect the views of the authors and do not necessarily represent the official policy of the AMA, the MJA or InSight+ unless so stated.
Subscribe to the free InSight+ weekly newsletter here. It is available to all readers, not just registered medical practitioners.
If you would like to submit an article for consideration, send a Word version to mjainsight-editor@ampco.com.au.

 more_vert
more_vert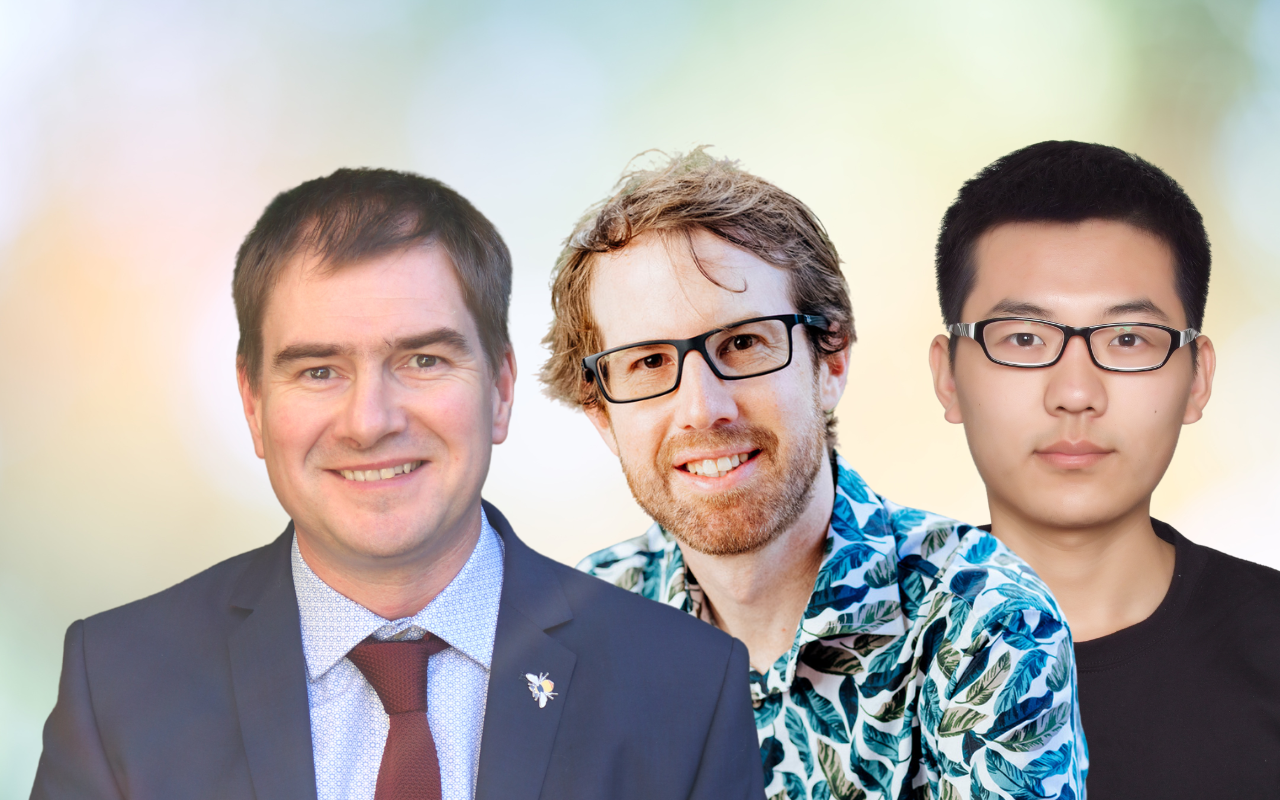
Thank you very much for your interest in our work. You are absolutely right— in Australia, veterinary antibiotics account for a significant portion of total antimicrobial use, even exceeding that of human antibiotics. As such, the use of antibiotics in livestock production and the reuse of animal manure in agriculture have profound implications for environmental health and the spread of antimicrobial resistance (AMR).
Australia enforces strict regulations on antibiotic usage. Many antibiotics are clearly designated for either human use (e.g., all quinolone antibiotics, linezolid, vancomycin, minocycline) or exclusively for veterinary use (e.g., tylosin, tulathromycin, sulfamethazine). Thus, the type of antibiotic can often indicate whether its source is human or animal.
In fact, according to our research, the proportion of animal-derived antimicrobials in municipal wastewater is minimal—virtually negligible. This is because wastewater from most livestock operations does not enter the municipal sewage system but is treated on-site through independent systems. Our study also found that antibiotics correlated with socio-economic factors are exclusively those intended for human use.
As the commentator rightly pointed out, given the substantial use of antibiotics in the livestock sector, understanding antibiotic residues in livestock waste and their environmental impact is crucial. In our recent research, we analyzed antimicrobial residues in wastewater from pig, cattle, sheep, and poultry farms across Australia. We found that the antibiotic profiles in these agricultural effluents differ significantly from those in municipal wastewater. Going forward, we will continue to investigate the use of antibiotics in the livestock industry and their environmental implications.
Once again, we sincerely appreciate your attention to the issue of antibiotic use and AMR in Australia.
These studies are very important.
I do wonder how much of the antibiotics in water comes from farms, cows, chickens, pigs?
Animals grown for food production would get the largest percentage of antibiotics.
(to help them to grow faster and fatten up, and prophylactically to avoid them becoming unwell
due to overcrowded conditions.)
Manure from these animals then may be further used as fertilizer onto crops/gardens- and further washed into creeks and the sea. Resistant bacterial strains then colonise humans which also then spread to water, or just get into the water.
How can we tell how much of the antibiotics use/resistance is coming from humans and how much
from animals? By removing antibiotics used for animals who are well, we would actually remove the largest source of
inappropriate antibiotic use.