Despite ongoing efforts to improve the communication of medicines information across the health system, medication errors at transitions of care persist. Each year in Australia, 250 000 hospital admissions are due to medication-related errors, costing our healthcare system an estimated $1.4 billion. More than half of medication errors occur at transitions of care.
The Australian Commission on Safety and Quality in Health Care recently released the Medication Management at Transitions of Care Stewardship Framework, which has the potential for real improvement and impact. The Framework is designed to reduce medication-related errors and hospital readmission rates for patients who are transitioning between hospital and primary and aged care settings.
The Framework is the first of its kind both nationally and internationally. It applies the lessons of prior antimicrobial and opioid stewardship programs, including focused governance and multidisciplinary coordination, and supports increasing digital maturity to achieve data quality and communication-focussed care across settings.
The Framework offers a stewardship model to achieve comprehensive medication reconciliation, timely discharge planning and collaborative post-discharge medication review and liaison. It comprises four elements:
- governing committee;
- multidisciplinary stewardship team;
- medication management activities; and
- monitoring, evaluation and reporting.
These elements can be tailored to the hospital’s local context and integrated into existing safety and quality frameworks. The approach is underpinned by effective communication between clinicians, person-centred care and digital enablers.

A risk-based approach to optimise medication management
The hospital-based Framework optimises medication management of patients and prioritises those who have been identified as high risk for medication misadventure. This includes people who are over 65 years old, take five or more medications or take a high-risk medication, and those with multiple prescribers for their medications.
The risk-based approach prioritises identifying high-risk patients at the time they are admitted to hospital. It also targets interventions focused on priority areas identified by health services’ own needs analysis.
Many hospitals already have systems in place to mitigate risk of medication error – but error rates persist. As clinicians, we appreciate that patients who are at high risk are often those who also have complex care arrangements across various health care providers and interdisciplinary teams, highlighting the importance of proactive communication.
For health service organisations, this Framework presents a prime opportunity to strengthen existing organisational approaches, processes and clinical practice. It calls upon hospital clinicians and health managers to take action to strengthen communication with the primary and aged care sectors – and highlights the enabling role of digital solutions in achieving this goal.
Digital enablement to support Framework adoption
Digital tools and technologies are transforming health care for all Australians. The Framework leverages several initiatives from the National Digital Health Strategy 2023–2028 to enable seamless information exchange, and recognises expanding national efforts driving improvements in health infrastructure and interoperability.
Digital maturity matters when it comes to realising the full benefits of Framework adoption. Embedding interoperable digital tools is especially important to streamline communication about medicines use across settings. It is also vital that high quality medicines information can be reliably interpreted across electronic medication and medical record systems.
The Commission recognises that digital maturity and implementation capability vary across Australia. While health services are at various levels of digital maturity, we urge clinicians to consider how digital tools and technologies could optimise the management of medicines for patients at care transitions. Many of the activities highlighted in the Framework can be streamlined or occur by default with good digital tools and technologies, when used consistently.
In practice, this means that a health service organisation ensures their digital systems are easily accessed by different members of the care team. It means having interoperable prescribing and dispensing software that talk to each other. It also means using standardised electronic discharge summary templates to complete discharge summaries and uploading these to a patient’s My Health Record (MHR).
Call for a collaborative multidisciplinary effort
Is there an opportunity to embed the principles for safe and high-quality transitions of care where you work?
The Framework empowers clinicians to lead the implementation of the Framework, tailoring their approach to their hospital’s local context, with the support of their leaders and policy makers.
Quality improvement based on the Framework is intended to be incremental. The Framework is presented in such a way that allows clinicians and health managers to familiarise themselves with the four core elements, while identifying specific local needs and priority areas. This enables its use as a tool to advocate for certain focus areas to be addressed within an organisation.
As described in the first element, the Framework highlights the importance of identifying the most appropriate committee – within the hospital’s existing governance structure – to assume responsibility for medication management at transitions of care stewardship.
The second element outlines how to appoint a multidisciplinary team of clinicians to champion stewardship across the facility and educate the workforce, to assist with the implementation of quality initiatives and minimise barriers to change.
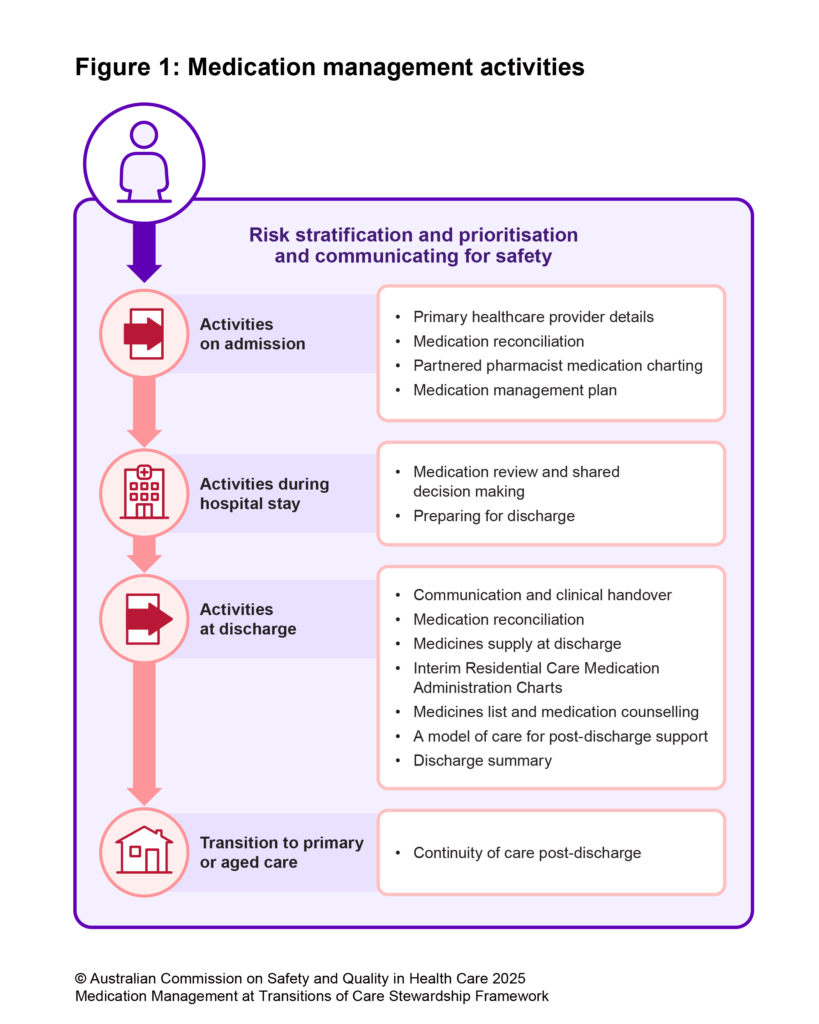
Recommended activities in the third element, to support safe and high-quality medication management – from admission to hospital and then to post-discharge follow-up – are already standard practice for many hospitals. However, some hospitals may benefit from identifying which activities can be considered for priority improvement to achieve local benefit (see Figure 1).
One recommended activity is partnered pharmacist medication charting, in accordance with local state and territory legislation. This involves credentialed pharmacists working closely with doctors to chart medicines for administration – an approach that has shown significant reductions in medication errors and length of hospital stay.
The Framework emphasises that stewardship of medication management does not end at discharge. In addition to uploading high-quality discharge summaries to a patient’s MHR and delivering these to the patient’s GP via secure messaging, the Framework advocates for the hospital doctor to verbally relay key recommendations to the GP or practice nurse before a patient is discharged back into their care. This allows a conversation where significant medication changes can be identified and enables the GP to see the patient within days of their discharge to reduce risk of medication-related harm.
It also calls for establishing a model of care that facilitates access to collaborative comprehensive medication review services post-discharge. To achieve this, there needs to be clear communication processes, ideally digitally enabled, established between clinicians across the acute, primary and aged care sectors to support continuity of care.
Finally, the fourth element promotes continuous monitoring, reporting and evaluation of improvement initiatives against locally determined quality indicators.
Ultimately, the successful adoption and implementation of this Framework demands holistic change across the whole healthcare system.
By recognising a shared commitment to stewardship of medicines management at care transitions, there is a real opportunity for us to make a profound difference to reduce risk of harm from medication errors and improve patient outcomes.
Natalie Kahwajy is a Senior Project Officer, Digital Health at the Australian Commission on Safety and Quality in Health Care and a pharmacist
Rodney Ecclestone is a Program Manager, Digital Health (Integrated Systems) at the Australian Commission on Safety and Quality in Health Care
Dr Phoebe Holdenson Kimura is a Medical Advisor to the Australian Commission on Safety and Quality in Health Care and a general practitioner based in Sydney
The statements or opinions expressed in this article reflect the views of the authors and do not necessarily represent the official policy of the AMA, the MJA or InSight+ unless so stated.
Subscribe to the free InSight+ weekly newsletter here. It is available to all readers, not just registered medical practitioners.
If you would like to submit an article for consideration, send a Word version to mjainsight-editor@ampco.com.au.

 more_vert
more_vert
What about the ‘Aged Care Transfer Summary’ document that the Australian Digital Health Agency talks about so much?
Loading discharge summarise to My Health Record is so critically important, not only by Hospitals but also by Age Care Homes when discharging a resident for transfer into hospital. My mum was transferred from an aged care home to hospital. The home printed out 12 pages of detailed medical, personal, welfare and dietary details. Handed it to my brother who travelled with mum to the hospital. My brother handed the documentation to the triage nurse – who LOST the documentation. The family then had to guess the answers to the emergency department Doctor and Nurse enquiries. Because of the lost documentation and mums’ dietary constraints, my 87-year mum had no food for 30 hours after arrival. The family eventually demanded the hospital contact the age care home and obtain a copy of the medical history. her treatment was delayed because the hospital nurse lost the documentation. The hospital eventually requested the papers be faxed through from the care home. All discharge documents should be uploaded to My Health Record to save lives, time and money whilst improving patient experience and welfare.