The latest edition of the Australian Asthma Handbook offers pathways to improvement for asthma control, urging clinicians and their patients to move beyond over-reliance on SABA inhalers in favour of inhaled corticosteroid (ICS)-containing preventer inhalers.
Asthma control is an enduring challenge in Australia, where asthma claims the lives of over 400 people each year. These victims are the tragic tip of an iceberg of poor asthma control.
Of the nearly 3 million Australians living with asthma, research suggests nearly half have poor asthma control, more than half of whom make little or no use of inhaled corticosteroid (ICS)-containing preventer inhalers. There is a clearly a large opportunity for improvement in asthma care.
And yet despite decades of messaging about the importance of ICS, measures of preventer use stubbornly resist improvement.
Instead, many Australians with asthma rely on short-acting beta2-agonists (SABA). Research from community pharmacies finds that SABA overuse and poor asthma control are very common in people seeking over-the-counter SABAs. Further, many people lack understanding of the risks of SABA over-reliance.
In tandem with these clinical gaps, recent years have seen a growing awareness of the adverse environmental impact of inhaled respiratory medicines. This is principally due to the climate changing effect of the propellant gases in pressurised metered dose inhalers (pMDIs). SABA pMDI use is a key driver of such emissions, and is largely avoidable.
Change is needed. The latest edition of the Australian Asthma Handbook, launched in September, offers pathways to improvement for all the above challenges.

Getting tougher on the blue puffer
The Australian Asthma Handbook now recommends that no-one with asthma aged 12 and over should be treated with SABA alone. Now, every adolescent and adult with asthma should be prescribed ICS-containing treatment.
For the many Australians living with asthma who rely on SABA alone to manage their asthma, this recommendation may be unfamiliar. However, it follows in the footsteps of other countries. For example, the international GINA strategy has promoted this treatment strategy for some time, and so have British guidelines.
This is with safety is mind. Increasing reliance on SABA correlates with increased risk of death. The opposite is true of increasing ICS use.
The new Australian Asthma Handbook offers two options for initial treatment of adults and adolescents with mild asthma.
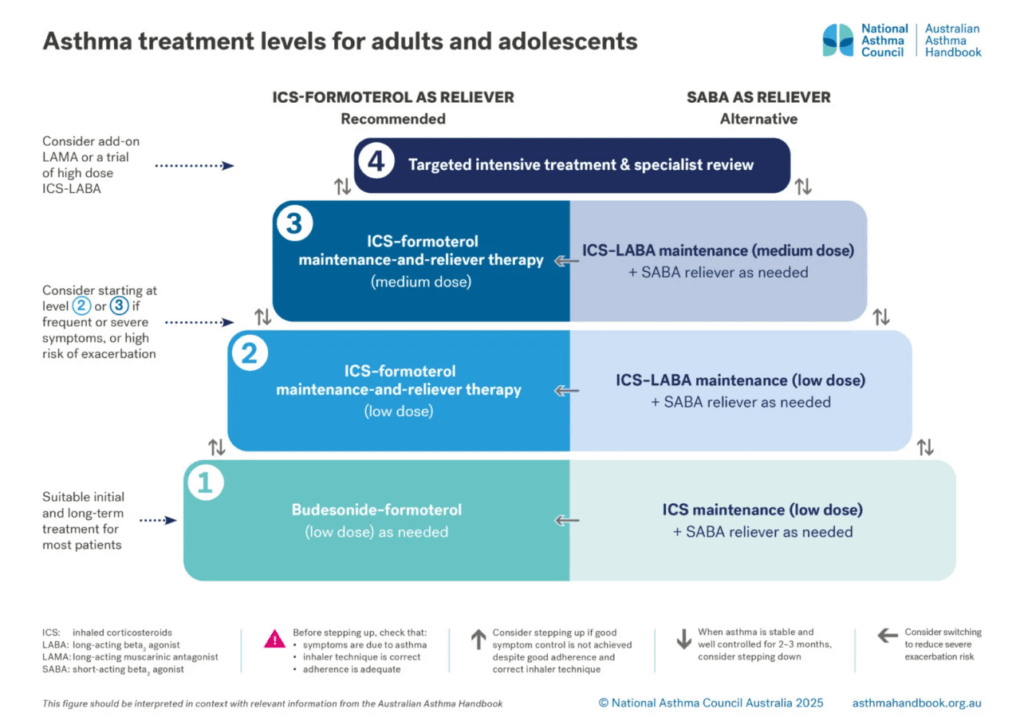
The recommended option no longer involves a SABA reliever at all. Instead, the use of budesonide-formoterol as-needed is the preferred first step. With this treatment, patients experience quick-onset bronchodilation from formoterol, but also benefit from the anti-inflammatory protection of the ICS. ICS-formoterol inhalers used like this for as-needed relief are called “anti-inflammatory relievers” (AIR). The preferred first step then is “AIR-only” therapy.
The alternative option is the traditional approach of a regular ICS combined with a separate SABA inhaler. This has the benefit of familiarity, but is no longer preferred, principally because adherence to the ICS component of such therapy is often disappointing. However, in a patient with established good adherence, continuation of such treatment is still appropriate.
Although it has been available on the PBS since 2020, not all prescribers seem familiar with AIR-only treatment in mild asthma. The intermittent use of ICS overturns the previous norm of ICS use needing to be regular. Several major trials have proven the safety and effectiveness of this strategy.
Highlights from the Cochrane review of ICS-only treatment in mild asthma include:
- AIR-only treatment, compared to SABA-only, more than halves the risk of exacerbations requiring steroids; and
- AIR-only treatment is at least as good at preventing exacerbation as the traditional regimen of regular ICS with SABA reliever, and possibly superior at preventing hospital admissions and urgent care presentations.
The advantages of this approach are not limited to individual asthma outcomes, but also include environmental benefits. When prescribed in dry powder inhaler (DPI) form, AIR inhalers can reduce the carbon footprint of asthma therapy by around 95% compared to strategies relying on salbutamol metered dose inhalers.
For people who do not achieve good asthma control with these basic approaches, the first step is to check device technique and adherence. If these are in order, stepping up to “maintenance and reliever therapy” (MART) is the preferred next step. This still involves ICS-formoterol inhalers (budesonide-formoterol or beclometasone-formoterol), but with regular use as well as as-needed doses.
There are further upward treatment steps for people with more severe asthma. A key point for GPs is when to refer to a respiratory physician. For people with inadequate control despite moderate dose ICS-containing therapy, referral will allow an eligibility assessment for biologic (monoclonal antibody) therapy. For eligible patients (with severe allergic or eosinophilic asthma) such therapy offers greater benefits, on average, than adding a long-acting muscarinic antagonist (LAMA).
Regardless of the level of therapy intensity needed, achieving good asthma control can help our patients to avoid the cumulative hazards of oral corticosteroid therapy.
A better future
Asthma is a common disease for which, at the population level, poor control is also common. This poor control has persisted for years despite health professionals working hard with traditional treatment approaches. Recent evidence has unlocked new treatment approaches that are safer, simpler, and more environmentally friendly. We hope the newly revised Australian Asthma Handbook will help lead a very necessary culture change in asthma prescribing.
Dr Brett Montgomery is a GP and member of the National Asthma Council Australia Guidelines Committee.
Clinical Associate Professor Debbie Rigby is Clinical Executive Lead of the National Asthma Council Australia.
The statements or opinions expressed in this article reflect the views of the authors and do not necessarily represent the official policy of the AMA, the MJA or InSight+ unless so stated.
Subscribe to the free InSight+ weekly newsletter here. It is available to all readers, not just registered medical practitioners.
If you would like to submit an article for consideration, send a Word version to mjainsight-editor@ampco.com.au.

 more_vert
more_vert
The webinar to launch the new Australian Asthma Handbook can be viewed here
https://vimeo.com/1119056831/a341eaf124
Hi would it be possible to have an education session for pharmacists doing full scope so as to give us tools to initiate the conversation.