At the Medical Deans of Australia New Zealand (MDANZ) Conference on September 4-5 in Newcastle, data from the Royal Australian College of General Practitioners (RACGP) and Australian College of Rural and Remote Medicine (ACRRM) was presented, analysing the association between medical school graduation and entry into general practice and rural generalist (GP/RG) training in 2025.
Using five years of university medical degree graduate numbers (2019-23) and 2025 ACRRM and RACGP enrolment data for their Commonwealth Funded training programs we analysed the absolute numbers of university graduates from each Australian medical school entering GP/RG training, and also calculated the proportion of graduates from each medical school choosing GP/RG.
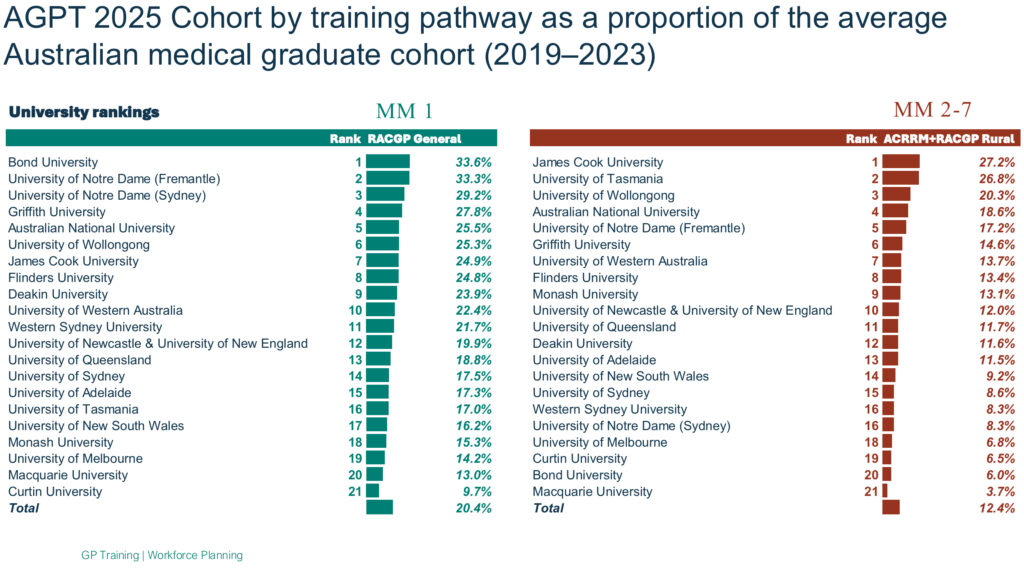
The results showed wide variation in the conversion from university graduation to GP/RG training, ranging from 16% to 52%. In terms of absolute numbers Monash University in Victoria, and the University of Queensland both contributed more than 100 graduates to GP/RG training from their large cohorts, while in terms of proportion, two universities had more than 50% of their average cohort size entering GP/RG training in 2025 — James Cook University in Townsville, and The University of Notre Dame Australia (Fremantle).
Through this university of origin analysis, we found nearly one third (32.9%) of the average medical school graduating cohort entered GP/RG training. This data contrasts with medical schools’ outcomes database (MSOD) which reports the career intentions of medical graduates at lower rates and declining — with the most recent report suggesting that only around 15% of medical school graduates intend to enter either GP or RG specialist training.

For too long, Australia has not been training enough GP/RG graduates to meet the growing needs of our ageing population increasingly living with chronic health conditions. This data provides some important insights into the differences across metropolitan, regional and remote training, and shows major variance in terms of the number of GP/RG trainees. There is a shift in intention between medical school graduation and actual choice of choosing GP/RG. Reasons for this warrant further investigation and could include internship and residency experiences, lifestyle considerations, employment opportunities, exposure to positive GP role models, or the availability of training places.
There is an increasing urgency to grow the Australian GP/RG workforce, which requires greater understanding of career choices for medical students and doctors at multiple points. The next part of this collaboration is to provide longitudinal analysis of trends in the university of origin. The current analysis has used an average over five years of each universities graduation data and may underestimate the graduate outcomes from newer medical schools such as Curtin and Macquarie universities.
This data may provide a mechanism to understand why some universities are producing more GP/RGs, and potentially recognise how they do this, or support them to do this more broadly. Further, the need for data spanning the entire lifespan of a GP/RG is also imperative to enable assessment of the various influencing factors leading to referencing and retention in metropolitan, regional, rural and remote medical care. This could be achieved through improved data linkage and analysis across MDANZ, medical schools, medical colleges, and the Australian Health Practitioner Regulatory Agency.
Dr Michael Wright (MBBS MSc PhD FRACGP GAICD) is a general practitioner, health economist and health services researcher based in Sydney. Dr Wright is the president of the Royal Australian College of General Practitioners (RACGP) and Associate Professor at the International Centre for Future Health systems at the University of New South Wales.
Dr Rod Martin (BSc, MBBS, FACRRM, JCCA, DRANZCOG (Adv), MAICD) is a Rural Generalist , currently working in primary practice in Armidale, as well as being a senior lecturer in rural medicine and critical care at the University of New England, and teaching medical students while practising as a visiting medical officer in anaesthetics, obstetrics and emergency medicine. Dr Martin is the current ACRRM President, has nearly 10 years’ experience as an ACRRM Council representative, been an ACRRM examiner for over 15 years, and contributed to curriculum development, including palliative care and rural point of care ultrasound.
The statements or opinions expressed in this article reflect the views of the authors and do not necessarily represent the official policy of the AMA, the MJA or InSight+ unless so stated.
Subscribe to the free InSight+ weekly newsletter here. It is available to all readers, not just registered medical practitioners.
If you would like to submit an article for consideration, send a Word version to mjainsight-editor@ampco.com.au.

 more_vert
more_vert
Well done – a useful repeat of work by Gerard Gill Deakin University 2016. However – the denominator is not a reasonable approximation for the purpose of the study. It suggests that graduates choose general practice at the earliest possible opportunity—PGY2 entering training as PGY3 and that these graduates are ‘the same as’ those who chose general practice later.
Given that our research demonstrated a significant shift during the prevocational years from a different specialty such that the PGY2 entrant was not reflective of the majority, this matters for universities that have in 2025 graduated only or mostly PGY2 and PGY3 doctors, and none of the PGY5 and PGY6 doctors.
In other words, it also needs to be shown when graduates actually enrolled successfully in the AGPT program by university. Any skewing across PGY entry level then needs to be described and interpreted accordingly. No doubt the reasons will be contextually diverse.
Thank you for an article of well presented data.
As for the mechanism to increase the supply of appropriately trained GPs/RGPs my simplistic suggestion is to restrict entry to Specialist Training courses to practitioners who have spent at least 2yrs (insert any appropriate duration) in General Practice. (duration should be long enough to convince practitioners to seriously consider staying in Primary Care.
As a now retired Specialist Anaesthetist I consider generalist experience, gained prior entering specialist training pipelines, of wholistic consideration of the patient and history taking, communication, focused investigation and broader issues of longer term implications for the patient, family and community to be extremely valuable insights and skills to be brought to any further specialist training programme. Professional growth time not wasted whether remaining in Generalist practice are transitioning to Specialist Practice.
There is also a longitudinal factor to this data, how long do doctors remain in rural or urban practice, and do they work part time or full time? The study does not address these questions, new entrants are fine but established long term GP’s are the gold standard.
In practice, there is a strong drift of rural doctors to urban settings after five years, and there is also a tendency for female doctors towards part time practice, so I would be wary of drawing too many workforce assumptions from this data.
My thanks also to the authors. What intention is there to determine how many of these home-grown Australian GP/RG registrars stay in MMM 2-7 once Fellowed? Doctors-in-training are all very well – but they ain’t credentialed for unsupervised practice until Fellowed. My question is, do they stay as Fellows …. or drift away again into other locations and/or pursue joint non-GP specialist vocation training programs?
do you have data on original place of residence (ie metro, rural, remote etc) as med students and current intention to undertake GP/RG training. Are student intakes from rural areas more likely to undertake RG training?
Interesting article. No mention of the continued de-fragmentation of general practice with pharmacy focused health care and prescribing., Nurse practitioner roles usurping GP roles. No mention of how many embark on the pathway of general practice and then cease only to pursue a speciality because the rural generalist pathway was restrictive and in some cases punitive. It also doesn’t help when politicians stand up holding a Medicare card stating this is all you need to see a general practitioner. The reality is that general practice pays poorly and the general public want it for free. Perhaps that is what health bureaucrats want for all general practice services to be delivered by the government. We all know how that ends.