Health care both contributes to and is affected by climate change. InSight+ spoke with researchers who recommend that Australia follow other nations and commit to considering environmental impact in healthcare technology assessments (HTAs).
Researchers argue that Australia should consider the environmental impacts of health care technology when approving technologies for the Medicare Benefits Schedule (MBS) or the Pharmaceutical Benefits Scheme (PBS).
According to the World Health Organization (WHO), climate change is expected to cause approximately 250 000 additional deaths per year between 2030 and 2050, due to malnutrition, malaria, diarrhoea, and heat stress. The direct damage costs to health are estimated to be $2–4 billion US per year, by 2030.
According to Health Care without Harm, if health care were a country, it would be the fifth largest emitter on the planet.

Mr Jake Williams is a PhD candidate within the School of Public Health and National Health and Medical Research Council (NHMRC) Clinical Trials Centre at the University of Sydney. He received the 2025 HEAL Scholarship from the Deeble Institute, the research arm of the Australian Healthcare and Hospitals Association (AHHA). Mr Williams authored the Deeble Issues Brief with the institute.
“HTA is the process we use to inform decisions about the value of health technologies,” said Mr Williams.
“The word ‘technology’ covers things including tests, devices, medicines, vaccines, procedures, and interventions. In Australia, the most well-known examples [of HTAs] are to inform decisions about whether a technology should be funded through the MBS, or the PBS,” he said.
“The process focuses on clinical and economic questions about the technology. Does it work? Is it safe? What does it cost? And other questions such as, are there unmet needs, or social or ethical issues?” he said.
Mr Williams said that Australia does not currently consider the environmental impacts of medical technologies in its HTAs.
“Guidelines for HTAs undertaken to decide on new listings on the MBS already allow environmental information to be considered — but this is not a requirement, and there is no evidence that it is happening regularly,” he said.
Health care and climate are connected
Mr Williams said that health systems and climate change are connected in two ways.
“The first is that climate is an urgent health problem. We are already experiencing record levels of health threats from climate change, and this is likely going to get worse unless we rapidly reduce greenhouse emissions in all sectors of the economy,” said Mr Williams.
“The second is that health systems themselves contribute to the greenhouse gas emissions causing climate change.”
“We know that the emissions of healthcare systems are big; globally they account for about 5% of total emissions.”
“To put this into perspective, healthcare emissions are higher than the aviation industry and, in most countries, healthcare is only exceeded by industries related to energy, transport, and construction.”
“Reducing healthcare emissions is a pressing priority, which is recognised by the Australian Government’s Health and Climate Strategy. It’s clear that the operation of the health system can contribute to a net-zero emissions economy,” said Mr Williams.
Clinical practice wants to act
Clinical practice accounts for 80% of emissions from the health care industry.
Mr Williams said that there is desire for HTAs to change and consider environmental impacts in health care.
“Clinicians want to act on climate change,” he said.
“Sustainable healthcare efforts have been supported by the Royal Australasian College of Physicians (RACP) and the Royal College of General Practitioners (RCGP). You can look at bodies like Doctors for the Environment Australia and the Global Climate and Health Alliance, which are very active in this space.”
Mr Williams said that doctors need support at the higher levels to enact change.
“We know that we ask so much of clinicians already, and I think that’s why system level decisions and actions can play such an important role.”
“While there is space for actions on an individual level, system-level changes — like changes to health technology assessment — will be less onerous on individual clinicians,” he said.
What needs to change?
Mr Williams worked with fellow researcher Adj A/Prof Rebecca Haddock, executive director of Knowledge Exchange at the Deeble Institute, to suggest changes to how the sector should account for environment.
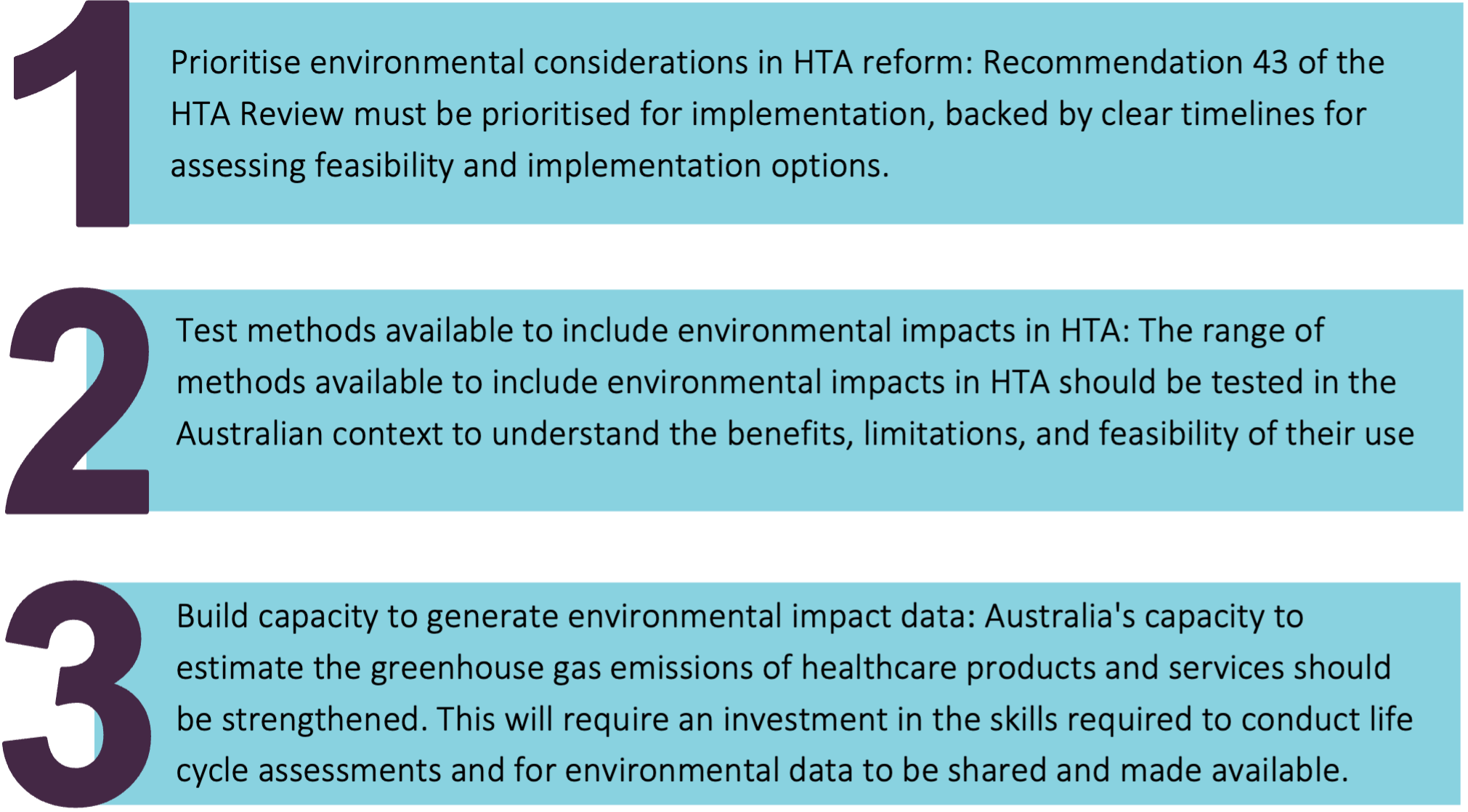
“There are three big things that need to happen for HTAs to consider environmental impacts in Australia, and we go into detail about these in our Deeble Issues Brief,” said Mr Williams.
“First, we need to prioritise environmental considerations in HTA reform. One of the recommendations of the recent HTA review was to explore how environmental impacts can be included in HTA, and this recommendation should be prioritised for implementation.”
The federal government’s recent HTA review included recommendations that the government, in line with the National Health and Climate Strategy, should investigate options in consultation with industry and other stakeholders during the assessment of cost-effectiveness by Australian HTA bodies, aligning with international best practice in comparable jurisdictions.
“Second, we need to test and agree to appropriate methods to include environmental impacts in health technology assessment. This should consider how to include environmental impacts, but also when we should do so,” said Mr Williams.
“Third, we need to generate, and build capacity to generate, data about the environmental impacts of health technologies.”
This month, InSight+ spoke with researchers highlighting the impact of climate change on antimicrobial resistance, and the benefits of reducing climate impact to antimicrobial resistance (AMR) containment.
InSight+ has also reported on greenhouses gases and hospitals, and asthma technology.
What changes might we make?
Mr Williams said that there has been movement in changing HTAs, and other countries have taken similar pathways to improve greenhouse emissions from health care.
“The UK and Canada have both committed to exploring how they can include environmental impacts in their HTAs,” said Mr Williams.
“Neither of these countries has finalised an approach. But it’s important that our efforts are consistent. Australia has an opportunity to lead in this space.”
“A logical scenario might be to consider environmental impacts as a ‘tie breaker’ when a new technology is not expected to have any health benefits or cost savings. In these scenarios, higher environmental impacts could be used as a reason to reject the application, and lower impacts could be used as a reason to support an application.”
“What remains difficult are decisions where health gains or cost savings are being weighed against environmental impact. Now, these kinds of questions are quite controversial, but I don’t think many are suggesting that otherwise cost-effective interventions should be rejected based on their environmental impact,” he said.
Mr Williams said that more research is needed to understand what trade-offs are acceptable to Australian decision makers and society.
Becca Whitehead is a freelance journalist and health writer. She lives in Naarm and is a regular contributor to the MJA’s InSight+.
Subscribe to the free InSight+ weekly newsletter here. It is available to all readers, not just registered medical practitioners.

 more_vert
more_vert