Patients with chronic conditions have better health outcomes with long term GP care from a GP who knows them, a new survey shows.
The value of continuity of care for Australian patients with chronic conditions and long term relationships with their general practitioner was highlighted in the results of the first ever Patient-Reported Indicator Surveys report (PaRIS).
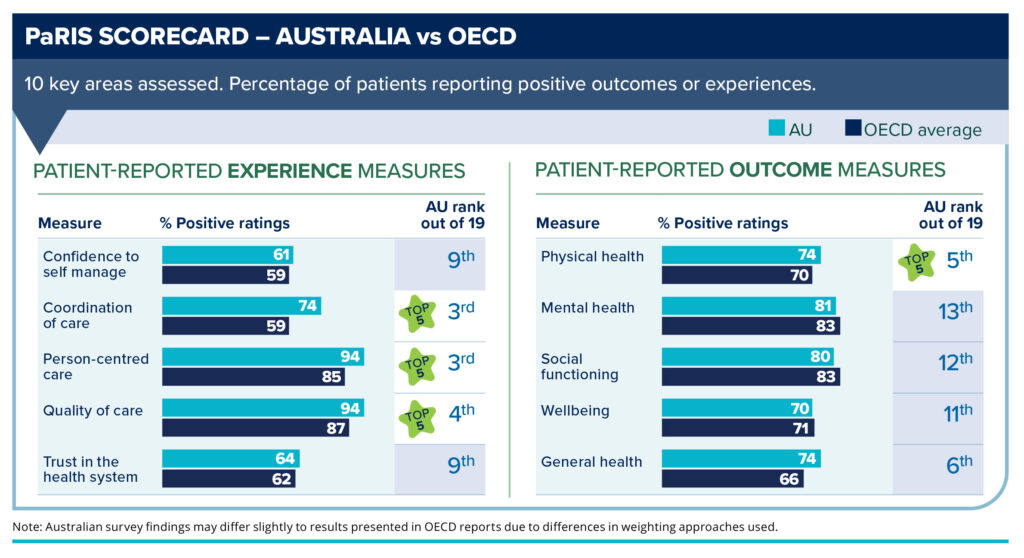
Health data from 107 000 patients with chronic conditions and 1800 practices across 19 countries were compared — with Australia holding up well internationally.
The landmark report is important because it gives a rare patient perspective on the health system, as PaRIS directly asked patients about their health experiences and outcomes.
Associate Professor Liz Marles is a practising GP and now Clinical Director with the Australian Commission on Safety and Quality in Health Care, which conducted the inaugural Australian report based on the PaRIS data. She says the results confirm what GPs have long known: that having long term relationships with patients leads to better health outcomes.

“I think the big takeaways for us here in Australia, as we were one of 19 [Organisation for Economic Co-operation and Development (OECD)] countries participating, is that overall our health system is performing pretty well in primary care,” Dr Marles says.
“We were in the top five for four out of ten measures, and, really pleasingly, three of those were inpatient experience measures. So that’s patients rating the quality of their care, whether it was person-centred and how well coordinated it was.
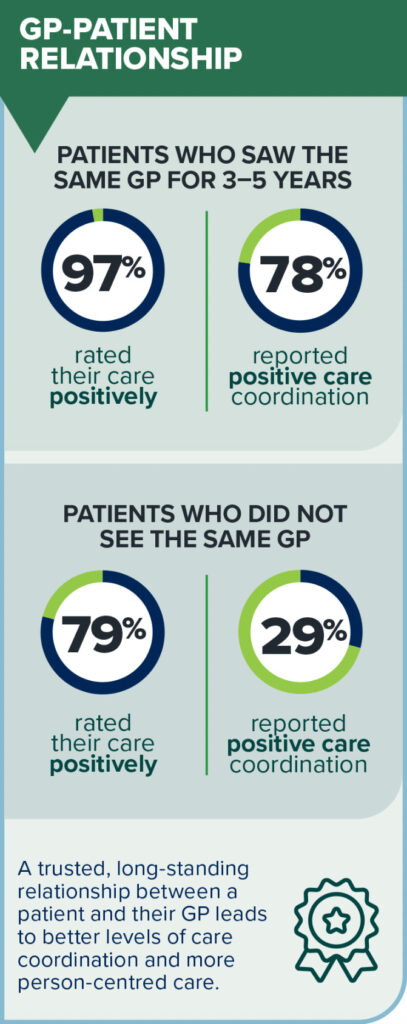
“So we’re really, really delighted to see those figures. And the other really big thing that came through was that continuity of care really matters. Seeing the same GP delivers definite health benefits. And the patients themselves recognise this.
“To actually see patients themselves reporting that they rate their care positively higher when they have seen the same GP for three to five years rather than those who don’t see the same GP is very affirming.”
Continuity of care matters
The Australian Commission on Safety and Quality in Health Care found that:
- 97% of patients who saw the same GP over three to five years rated their health care positively, compared with 79% among patients who do not have a usual GP;
- 80% of patients who saw the same GP for more than one year reported positive experiences of coordination of care, compared with only 29% of patients without a usual GP;
- 62% of patients who saw the same GP for most of their health care needs said they trust the health care system, compared with 43% of patients who did not; and
- 95% of patients who saw their GP for more than a year rated their care as good to excellent and 87% said they trust their GP.
Royal Australian College of General Practitioners (RACGP) President Dr Michael Wright says this provides strong evidence for further investment in the sector to ensure all Australians can see a GP who knows them.
“GPs are the experts in providing long term, whole-person, safe, and comprehensive care, and we need to make sure that that’s supported by our health system,” Dr Wright says.
Almost two-thirds (around 61%) of Australians live with at least one chronic health condition, such as high blood pressure, back or joint pain, or mental health conditions such as depression and anxiety.
“We’ve been calling for investment in Medicare that supports the kind of care patients with chronic conditions need, particularly the longer consultations that are vital for managing these chronic conditions well,” Dr Wright says.
Areas for improvement
One area of concern Dr Wright noted was that while a growing share of patients depend on support from their GP for mental health care, this is an area where Australia underperformed in comparison to other countries.
“It’s important that we avoid changes that might fragment care or reduce patients’ ability to get that care from their trusted GP when they need it,” he says.
Dr Marles agreed, saying that although Australia held up well compared with other OECD countries, particularly around person-centred care, there were concerning results regarding care plans.
“We know that even though GPs are doing care plans for around 50% of their patients with chronic conditions, only 25–35% of patients reported that they had a care plan,” she said.
“That care planning is fairly critical for chronic disease, and it also assists the patients to self-manage. And that was another area that came out very clearly, that patients who self-manage tend to do better.”
The report highlighted barriers that some people face with access and affordability of health care. Patients with lower levels of income reported both worse experiences and worse outcomes, as did those living in regional or remote areas compared with patients in cities.
Dr Marles says Australia’s unique geography does complicate this, but the report gives a great starting point to look at the challenges Australia faces in primary health care.
“We know that, for instance, 18% of people didn’t seek care because of difficulties travelling to see their GP,” she says.
“And similarly, 17% of people didn’t take medication or seek care because of the cost.
“So we know that they are important elements and barriers to care that need to be on the agenda when we are looking at health reform and how we can deliver safe, high quality, and equitable care to all Australians no matter where they live.
“One of the solutions to that might be telehealth, for instance. And that’s actually where we did incredibly well. Australia survey respondents were four times more likely to say that their GP offered video consultations than the OECD average. And of those 96% rated the telehealth care positively.”
She says the survey results provide important lessons and insights for GPs, policy makers, and patients.
“For the patient[s] themselves, I think that, whilst we acknowledge that there are a lot of challenges for people in trying to sometimes access a GP, it is worth pursuing because we know that ultimately if you can build that good relationship with a GP, it will actually deliver higher levels of satisfaction, but also better health outcomes overall.
“Ultimately, what we want is for people to not only survive, but to thrive.”
Nance Haxton was a journalist at the ABC for nearly 20 years. She’s also worked as an Advocate at the Disability Royal Commission helping people with disabilities tell their stories and as a senior reporter for the National Indigenous Radio Service.
In that time she’s won a range of Australian and international honours, including two Walkley Awards, and three New York Festivals Radio Awards trophies.
Now freelancing as The Wandering Journo, Nance is independently producing podcasts including her personal audio slice of Australia “Streets of Your Town”.
Subscribe to the free InSight+ weekly newsletter here. It is available to all readers, not just registered medical practitioners.

 more_vert
more_vert
**Commendation to Specialist GPs**
Specialist general practitioners holding **FRACGP** and **FACRRM** qualifications provide the backbone of Australia’s health system. Their training ensures breadth and depth of expertise, enabling them to deliver the **continuity of care** that underpins patient trust, coordination, and long-term wellbeing. When care fragments—pushing patients into emergency departments for primary care needs—our system becomes riskier and costlier. Supporting these expert clinicians is essential if we are to strengthen preventive health, reduce avoidable hospitalizations, and safeguard equity of access for both urban and rural populations.
**Expanding Virtual Primary Care**
To complement in-person continuity, Australia must expand **virtual primary care led by these specialists**. Properly integrated telehealth—delivered by FRACGP and FACRRM clinicians—has already shown high patient satisfaction and the ability to overcome geographic and mobility barriers. For vulnerable and rural communities especially, well-structured virtual care enables timely, relationship-based access to the same trusted GP, rather than episodic substitutes. Investment in this model will not only reduce pressure on hospitals but also extend the reach of specialist general practice, ensuring that all Australians benefit from safe, coordinated, and continuous care.
To all GPs holding FRACGP and FACRRM credentials: Your dedication to long-term, comprehensive patient care exemplifies the very best of general practice. The PaRIS patient survey strongly affirms what you already know—continuity matters. However, we must address systemic fragmentation in Australia’s health care. Hospital EDs should not substitute for your trusted care; instead, we must build systems that empower your specialist skill and foster long-term relationships. This includes better support for vulnerable and rural populations, and sustained investment in virtual care models-led by properly skilled qualified clinicians (not the inexperienced medical officer, or registered nurse-prevalent in hospital virtual clinics). In doing so, we ensure that patients not only survive but thrive, under the excellent care you provide.
Evidence based health policy has been replaced by political donation based policy so don’t expect these confirmatory insights to get any traction in the halls of power, despite their importance for wellbeing and productivity.
This study is further proof of the obvious. Continuity of care should be promoted and supported at every level. Yet we have national and State governments dismantling continuity of care by legislating extension of scope for less well trained health workers and subsidising urgent care clinics.