A new screening tool, The General Practice Sleep Scale, holds promise as a practical, real-world solution to obstructive sleep apnoea underdiagnosis in general practice.
Obstructive sleep apnoea (OSA) remains a prevalent yet under-recognised condition, with major implications for public health. Moderate-to-severe OSA affects approximately 6–17% of the general adult population, with increasing prevalence being observed in women (previously thought to be a male predominant disease). Left untreated, OSA contributes to hypertension, cardiovascular disease, type 2 diabetes, neurocognitive impairment, and increased work and motor vehicle accident risk. The societal burden of sleep disorders in Australia in 2019–20 is estimated at $35.4 billion (OSA $13.1 billion) due to health system costs, lost productivity and reduced quality of life.
Despite the high prevalence of OSA, case detection in general practice is low. One reason is that current OSA screening tools are either too time-consuming or too narrowly focused. The Epworth Sleepiness Scale (ESS), for instance, measures only daytime sleepiness and other important risk factors for OSA. Tools like the STOP-Bang and OSA-50 offer broader risk profiling but can flag many false positives or require physical measurements that are not always feasible to administer in a busy clinical practice. Moreover, primary care physicians are burdened with competing priorities and time constraints. Consequently, primary care clinicians can often underutilise these existing OSA screening tools, resulting in missed opportunities for diagnosis and intervention for OSA.
Australian guidelines for direct referral for a sleep study rely on combinations of these existing screening tools, such as an ESS result ≥ 8 plus either a STOP-Bang result ≥ 3 or OSA-50 score ≥ 5 or Berlin Questionnaire result of “high risk”. However, the inconsistency in these tools’ predictive value and their limited practical use in primary care, suggests an urgent need for a more streamlined, clinically relevant screening approach. Moreover, it is reasonable to speculate that a recommendation to include multiple/complex tools in the Australian guidelines could be due to lower confidence in the clinical validity of any single tool in general population perspective.
The General Practice Sleep Scale
The General Practice Sleep Scale (GPSS) has recently been proposed to address these gaps. Published in the Sleep Medicine journal (2025), the GPSS is a newly developed nine-item screening tool designed specifically for use in primary care settings. It integrates:
- demographic risk factors: age, sex, BMI, neck circumference;
- sleep symptoms and comorbidities: snoring, witnessed apnoeas, unrefreshing sleep, daytime sleepiness; and
- the presence of hypertension, diabetes, heart disease or depression.
Each item contributes to a cumulative score (0–22), stratified into low (0–7), moderate (8–13), and high (≥ 14) risk for OSA. Validation against in-laboratory polysomnography in a 159-patient Australian cohort revealed strong discriminatory performance (Figure 1).
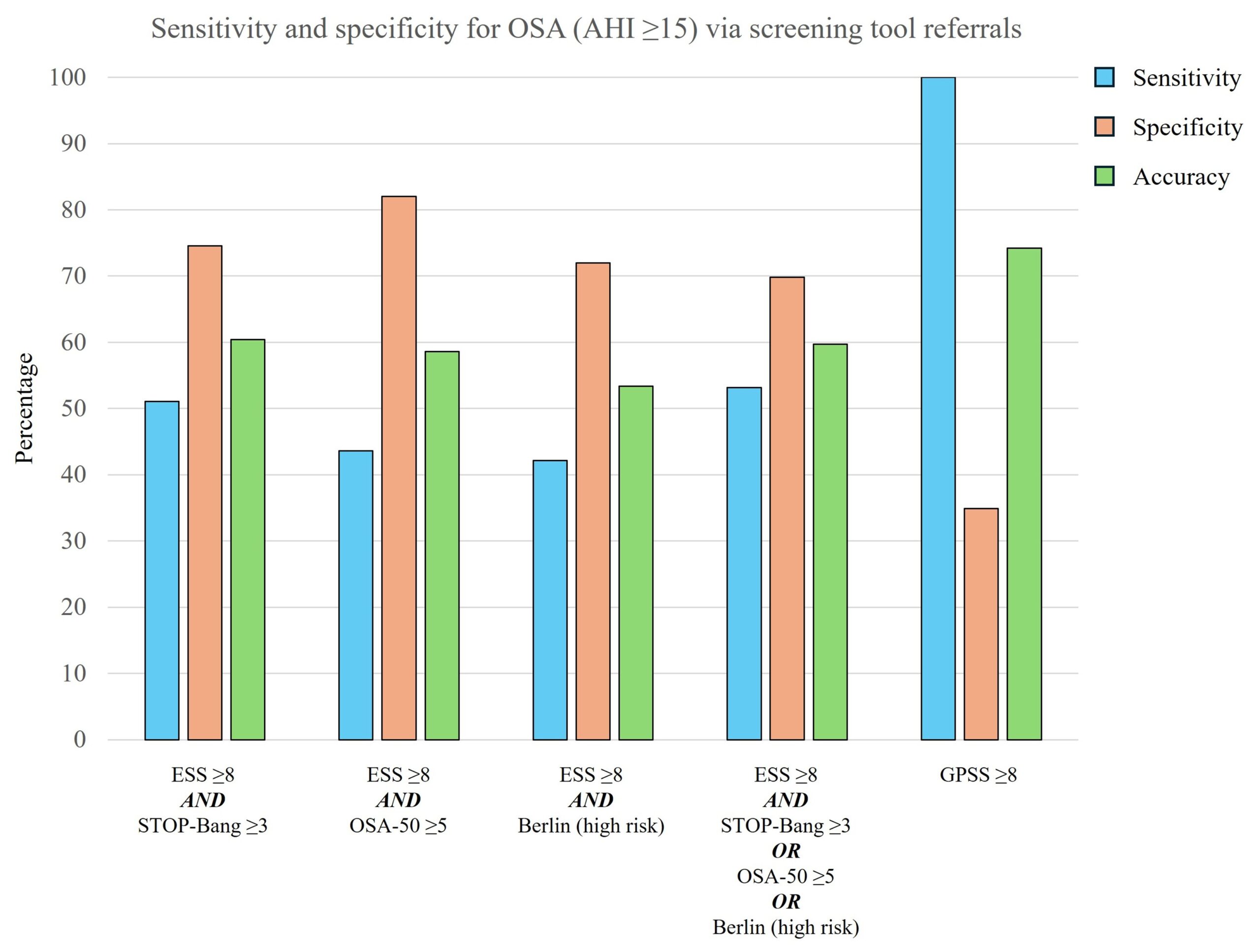
The GPSS showed 100% sensitivity for moderate-to-severe OSA at a threshold of ≥ 8, notably outperforming the ESS, OSA-50 and Berlin tools, and marginally exceeding the STOP-Bang test. While specificity was lower (≈35%), this is expected and acceptable in a screening context where the goal is not to miss at-risk individuals. Moreover, the GPSS also correlated closely with OSA severity based on AHI (Apnoea-Hypopnoea Index: an index to assess the severity of OSA) (Figure 2). Notably, 81% of patients with high GPSS scores (> 13) had moderate-to-severe OSA. In contrast, patients with low scores (0–7) were highly unlikely to have clinically significant disease. This robust stratification can support clinical decision making and streamline referrals for diagnostic testing, if appropriate.

A promising new tool
The GPSS (GPSS online tool, Figure 3) holds promise as a practical, real-world solution to OSA underdiagnosis in general practice and in the general population self-assessment context. Its simplicity and ease of administration require no complex calculations or physical examinations, which means it can be completed by patients in the waiting room or via digital pre-screening or with help from a practice nurse consultant. Its total score immediately informs triage decisions, enabling a targeted approach for the primary care physician to implement management, including undertaking further investigations such as sleep study referrals.
As with any new tool, further external validation is essential. The current evidence comes from a single-centre Australian cohort and future studies should assess performance across diverse populations and settings. To further support the use of the GPSS tool in general populations, a more recent retrospective assessment in a larger sample of 3959 individuals (conference abstract, SLEEP June 2025, Seattle, Washington, USA), which is yet to be peer-reviewed, showed a positive trend favouring the GPSS tool. Hence, only time will determine if the GPSS tool could be integrated into electronic medical records, Medicare pathways, and chronic disease management frameworks to improve early detection and reduce the burden of untreated sleep apnoea. Nonetheless, the initial findings are encouraging: the GPSS may offer a more efficient, accurate and feasible way to identify OSA risk in primary care than any existing alternative.

Dr Himanshu Garg is a respiratory and sleep specialist on the Gold Coast, Queensland, Australia.
Dr Timothy Howarth is a researcher for Darwin Respiratory and Sleep Health at Darwin Private Hospital and a post-doctoral researcher in the Sleep Technology and Analytics Research group at the University of Eastern Finland and at the faculty of health Charles Darwin University, Darwin, Northern Territory, Australia.
Professor Subash S Heraganahally is the head of the department of respiratory and sleep at the Royal Darwin Hospital, director of Darwin Respiratory and Sleep Health at Darwin Private Hospital and a professor in the faculty of health Charles Darwin University, Darwin, Northern Territory, Australia.
The authors do not work for, consult, own shares in or receive funding from any company or organisation that would benefit from this article, and have disclosed no relevant affiliations beyond their academic appointment.
The statements or opinions expressed in this article reflect the views of the authors and do not necessarily represent the official policy of the AMA, the MJA or InSight+ unless so stated.
Subscribe to the free InSight+ weekly newsletter here. It is available to all readers, not just registered medical practitioners.
If you would like to submit an article for consideration, send a Word version to mjainsight-editor@ampco.com.au.

 more_vert
more_vert