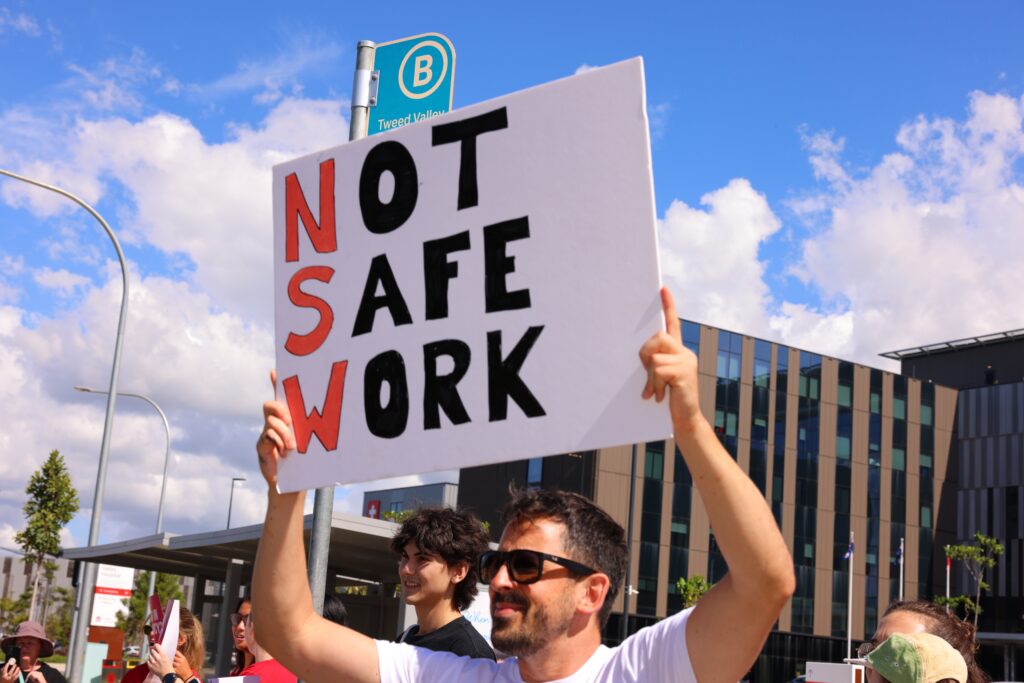
Junior doctors in New South Wales have long decried what they describe as unsafe working conditions and unequal pay. In February, junior doctors went on strike after a leaked email referred to the group as “marshmallows” for questioning working hours. Recently, the NSW government released its report from the Special Commission of Inquiry into Healthcare Funding, which calls for further efficiencies and funding.
InSight+ spoke to advocates to ask about working conditions, and what the report might change.
Earlier this month, junior doctors spoke to the ABC about what they say are still unsafe working conditions for doctors and patients. In the same report, Professor Jeffrey Braithwaite, a member of the inquiry’s expert panel, said that health care in general was like a “black hole”, that couldn’t be filled.
“There’s a case for them to be paid more, but after that you just reckon you deserved it, and that’s what you’re worth now — so it’s only a sugar hit,” said Prof. Braithwaite.
Negotiations between Premier Chris Minns’ government and advocates have hit a stalemate, but junior doctor and student doctor advocates say conditions must change.
Tom Morrison, Australian Salaried Medical Officers’ Federation (ASMOF) Junior Vice President, has been representing junior doctors in meetings with the government, and doesn’t agree with Prof. Braithwaite’s assessment.
“I think it’s a lazy argument to say more money won’t fix the problem. It’s like saying more petrol won’t allow your car to go further. If the tank’s empty, you need more petrol. And we’ve been running on fumes for years,” said Dr Morrison.
It’s about safety, not just wages
Dr Morrison says that working conditions are beyond reasonable and have been for years.
“When you push individuals to work beyond what they’re capable of doing and then put them in extreme environments where they’re making life-and-death decisions for patients, things get unsafe. In my case, it’s doing very large periods of on-call work and being constantly sleep deprived,” said Dr Morrison.
“If you’re flying a plane, you have mandatory rest periods. And if you haven’t met those safety thresholds, it doesn’t matter if there’re two hundred passengers waiting on the tarmac – the plane’s not taking off,” he said.
“Whereas in medicine, it’s the reverse – we have to do it anyway,’” said Dr Morrison.
Dr Morrison said that while wages are important, the main issue is still safety.
“There are no minimum safety standards that are enforced in New South Wales, or about the number of hours you can work in a row. Also, NSW doctors are paid 30% less than doctors in the rest of the country,” said Dr Morrison.
“That’s why a traditionally mundane, restrained group like the medical profession has come out in force with 6000 people striking,” he said.
Dr Morrison said that he has been happy with the public’s support.
“People agree that you shouldn’t be working for 30 hours in a row and making life-and-death decisions,” said Dr Morrison.
Morrison said that the pandemic created more work and a higher degree of care for the average patient.
“Due to the pandemic, with people leaving the system, we’re doing more with less. But the funding to catch up with that has not been appropriately matched,” he said.
The Commissioner’s report
The NSW Government recently released the report from the Special Commission of Inquiry into Healthcare Funding.
“The Commissioner has said the system has been woefully underfunded for public expectation and has been for years,” said Dr Morrison.
The report does not support the idea that further funding would be futile, rather suggesting that while improved efficiencies are required, the system needs further and sustained funding. It includes 41 recommendations for health workforce development, education and training, and funding and procurement, suggesting significant re-evaluation of the current systems that would improve working conditions.
Writes Commissioner Justice Richard Beasley, “If universal health care is the aim of the NSW public health system, at least parts of that system are underfunded. They have been for some time.”
Medical students feel “disposable”
Melody Ahfock is the President of the Australian Medical Students’ Association (AMSA), which represents over 18 000 medical students across Australia. Mr Ian Burton is President of the NSW Medical Students Council (NSWMSC).
Both say that working conditions are causing students to look outside of NSW when thinking about work.
“Fundamentally, this is about the way the government, health care, and to a degree the public, view junior doctors — which is disposable, effectively,” said Ms Ahfock.
Ms Ahfock agrees that current working conditions for junior doctors would be illegal in other industries.
“There are a lot of studies showing the correlation between tiredness and the equivalence of a high alcohol blood volume. Essentially, tiredness is similar to working under the influence,” she said.
“The cycle of abuse is being perpetuated by more senior health staff,” she said.
“The Victorian intern, for example, in 1992 would have been paid about $76 000. That’s the same as a current NSW doctor in 2025, and the equivalent purchasing power today would be $173 000,” said Ms Ahfock.
“But ultimately this isn’t a pay dispute. This is a dispute about patient and doctor livelihood,” she said.
Mr Burton is a student at UNSW. He says that his fellow students are looking outside of NSW.
“Obviously, pay isn’t the be-all and end-all, but it’s a consideration,” says Mr Burton.
“Junior doctors are given an unreasonable amount of work. And in New South Wales, you’re being paid less to do it. That extends to working extremely long shifts, being told not to drive home, because it’s unsafe. [Driving unsafely] shouldn’t be a condition of employment,” he said.
Mr Morrison agrees that attitudes to junior doctors “toughing it out” are no longer automatically tolerated.
“There’s this idea that junior doctors should suffer through the early years because they’ll be well paid later. But more and more, I see that the public isn’t buying that. They want doctors to be well enough to care for them,” said Dr Morrison.
Hope for better negotiations
Dr Morrison said that he has not seen much movement during negotiations.
“We’ve had over 15 meetings with the NSW Government. And every time we meet with them, their stance has been completely adversarial. And it becomes disheartening when they frame it like doctors are demanding luxury,” said Dr Morrison.
“We’ve been very open to thinking outside the box. But their attitude has been that the system can’t be changed — and that’s just not true,” he said.
Dr Morrison is hopeful that there will be a way to get better conditions for junior doctors.
“I’m optimistic that the government will realise that this is not a simple pay dispute, that it’s about the nature of the health system,” he says.
“The hope is that once the public truly understands how unsafe things are, they’ll support change. And I think that’s already happening.”
Recently, the World Medical Association has said that it is updating its Statement on Physicians’ Wellbeing. The move is largely in response to unprecedented pressure being put on physicians after the pandemic.
Subscribe to the free InSight+ weekly newsletter here. It is available to all readers, not just registered medical practitioners.

 more_vert
more_vert
It is naive to seem surprised this is still happening. Medicos must cover potential emergencies 24/7/365. To provide safe working conditions for everyone is beyond the funding capacity of most states. There probably have been further studies since then, but I recall someone tried to estimate the cost of providing safe doctor working hours in the state of Maccechusetts in the 80s – including on call emergencies for the likes of anaesthetists and surgeons, and came up with 2 billion per year (!!). It’s easier for those with home or relationship support, but overall harder for young women.
Having moved on to rural consultancy being available 80 to 120 hours per week, I must say it doesn’t necessarily get any easier
It’s important to keep fighting – what else can you do? The bureaucrats will calumniate and belittle you for trying, and push you right to the edge (I.e. force you to leave your sick patients and walk out) so you have to face that issue.
Good luck!
“There’s a case for them to be paid more, but after that you just reckon you deserved it, and that’s what you’re worth now — so it’s only a sugar hit,” said Prof. Braithwaite.
What an extraordinary analysis !
Not sure if it is apres Pontius Pilate , Marie Antoinette or Nero !
You need to go on strike again and again until this is fixed. Dont back down! Junior doctors need support. Don’t be silenced don’t back down. If you do you are back to square one.
It is very disappointing that safe working conditions for junior doctors is still an issue. It is even more disappointing that there are still dinosaurs out there who think that they need to “harden up” because they did it the hard way. I was a junior doctor in the late 90s and early 2000s. It is not ok that I was curled in a chair 15 minutes before the end of a 16 hour shift hoping and praying that no-one would call me to see a patient before my shift finished because I had no brain power or emotional capacity to do any more – and would have to be back for the next shift in less than 8 hours. It is not ok that I would hallucinate while driving home because I was so tired, fall asleep while waiting at roadworks, or wake up veering across the lanes after a microsleep. It is not ok that I felt suicidal and wondered why I bothered studying so hard to get into this profession in the first place. It is definitely not ok that this is still the case for junior doctors. Whilst it is true that I learned a lot being on call as a junior doctor, this learning should not be at the expense of patient and doctor safety. Junior doctors, please know that most senior doctors that I know are there for you and will support you. Please call on us for help if you are overwhelmed – we don’t necessarily know what is going on for you if you don’t tell. us. I have certainly divided and conquered the workload with my on call fellow when things were out of control, and together we got done what needed to be done.
If you’re told you are unsafe to drive home, at what prior point did you become unsafe to doctor?
Unbelievable that this is still happening in 2025. It’s a combination of pay AND working hours. If you can pay a doctor all of $38 per hour to cover scores of patients on wards, and work them >14 hours per day, there’s little incentive to change the structure. Pay parity and some obvious changes to shift length and structure are both needed to make these jobs conform to normal principles of safety and equity.
It’s common to have 14 hour shifts Saturday and Sunday – probably 15-16 hours in reality, so there are people working almost a fulltime working week’s equivalent in the weekend alone. This isn’t even on call, this is constant work. These could be split into 7 hour shifts. Doctors are at work as long as 12 days in a row. The fatigue and demoralization is clearly leading to loss of valuable staff from NSW and probably from the medical profession altogether.
To commenter Andrew Hallam:
What point exactly are you trying to make? Arguing that patients deserve lower quality care from sleep deprived doctors working unsafe hours just because your patients were subjected to the same decades ago is an absolutely wild stance to take. Make sure you tell your loved ones you’re ok with them being resuscitated by/operated on/cared for an exhausted overworked doctor who cannot perform at their best just because you did it to your patients in the 80s. Shame on you for not supporting today’s generation of doctors in training in advocating for system improvements to provide higher quality care.
Harden up! Good training requires long hours. My job with the NHS in mid 1980s was 88 hours a week. Yes it was tough and I was sleep deprived. But the morale of the team was high and the experience fantastic. Medicine was never a 9 to 5 job and nor should it be.
I recall “safe working hours” becoming identified as an issue in 1986 – nearly 40 years ago! Why is this still happening? In our major tertiary public hospital registrars are doing 60 hours weekend on call 6pm Fri to 6am Monday and then having to drive 90 minutes to a regional clinic for an 8am start – barely time for breakfast, and certainly not sleep! I have no doubt that patients are being at least compromised and at worst, are dying as a result of sleep deprivation induced poor management decisions, I am sure that chronic sleep deprivation is also contributing to the mental health issues and suicide rate of our younger doctors – the disgusting labelling of these bright young minds as “marshmallows” says it all about the attitude of the administrators who need to be held personally responsible.
I was the President of the RMOs section of the PSA in 1974 and we took the Health Commission of NSW to Arbitration. The 40 hour week was granted but 51 years later is still not observed. We also won a 95% increase in pay which made for NSW the highest paid State for a while. If saddens me to read of the problems that the RMOs are now facing..
By the way we only got to Arbitration by holding a strike. For that I gave up my ambition to work in a Sydney Teaching hospital so worked in rural and regional hospitals around Australia. I loved it so kept going until age 76 and the end of the COVID epidemic.
Professor Jeffrey Braithwaite has qualifications in health care administration – the bureaucratic part of health systems. The very domain us clinicians allege is making health care unaffordable and clinician’s life miserable and – most importantly – endangering our patients.
Nations who lead in health care outcome such as Norway have demonstrated for decades now that you can achieve better outcome with less money – and at the same time treat and pay clinicians well, and enforce safe working hours and conditions. So, it is doable. It is doable for LESS money. You can both have your cake and eat it too. The evidence is there. Has been for a long time now. The anglosphere keeps ignoring it.
Alas, instead the health bureaucrats defend their little empires, the discriminative several tier health system, and the horrendously wasteful state/federal divide in health care. The bean counters in NSW never batted an eye at throwing hundreds of millions at (not all that clinically useful and definitely not user friendly ) software, just so that they could get some numbers to play with (that are mostly wrong, because the atrocious user interface will invariably lead to wrongful data capture), but always shirk from deploying reasonable staff numbers at reasonable pay for the expected case load.
Quality and cost effective care cannot be delivered by an exhausted sleep deprived work force, where underpayment contributes to poor staff morale. Especially not when bureaucrats constantly interfere micro-managing the clinical decision process and increase our workload with nonsensical administrative burdens. I walked away from NSW health in 2017, and have no regrets.
I am not sure where the pay of 76000 for interns in Victoria in 1992 came from. When I worked as an intern in 2009, our hourly rate was 23 dollars. You probably should clarify if the pay is with overtime / after-hours or not.
This was a problem in 1965 when I was an internet. We approached the AMA and their attitude was that all previous generations had passed through this system so it was pointless to bring it up. Looks as if nothing has changed. I remember doing 48 hour shifts often, at least weekly. It was unsafe then, so I hope things have improved. I wish the present generation luck but wont hold my breath.
Health care is not a “black hole” but it is a massive challenge thanks to increasingly unsustainable demand. On one side the public now have massive expectations of unconstrained access to expensive “free” healthcare, and on the other side we have politicians who promise to provide it. Junior doctors in particular are the ones who are required to bridge this chasm, and are correctly declining to destroy their lives engaging in this charade. A solution will require realism and honesty on the part of patients and politicians, and acceptance of more community based palliative care and less heroic hospital care.
I see Braithwaite has never worked as a medical practitioner, condescending metaphors abound