“I know my patient needs more than just medication, but I don’t know what else to offer.”
This common sentiment among health care providers reflects a critical gap in medical education: the ability to address social determinants of health (SDH) effectively. While our health care system aspires to deliver holistic person-centred interprofessional care, the reality often falls short, with practitioners trapped in a more siloed and reactive biomedical paradigm that overlooks crucial social and environmental factors that affect outcomes.
SDH are non-medical factors that impact health and wellbeing outcomes, ranging from social isolation to financial and housing issues. They are associated with poor long term health outcomes and potentially interfere with engagement in preventive behaviours. One example gaining attention is social isolation and loneliness. Prolonged periods of social isolation and loneliness can negatively impact a person’s mental, physical and social wellbeing, leading to increased risk of developing anxiety and depression, dementia, cardiovascular disease and early mortality. Together with increasing use of health services, loneliness is also an independent risk factor for early nursing home admission.
| Loneliness: A subjective, unwelcome or distressing feeling of a lack of connection to other people, alongside a desire for more or more satisfying social relationships. Social isolation: Having objectively fewer social relationships, social roles, group memberships, and infrequent social interaction. Social connection: Having a variety of relationships (from close personal ties such as family and friends through to weaker ties such as acquaintances and strangers); relationships you can rely upon for support; and relationships that are trusted, high quality, and satisfying. |
Loneliness prevalence is significant in Australia. One in three (32%) Australians report experiencing moderate loneliness, and one in six (17.5%) report experiencing severe loneliness. Social connection is protective against loneliness and social isolation.

A solution: social prescribing
There are many ways to encourage social connection, with social prescribing being one method that is gaining increasing attention. Social prescribing is “a means of enabling health care professionals to refer people with non-medical health needs to a range of local non-clinical services”, and allows for integration of primary health and social support within the community. Social prescribing has been shown to improve wellbeing, loneliness, social connectedness, self-confidence and general health; and is associated with reductions in health care appointments and emergency department visits.
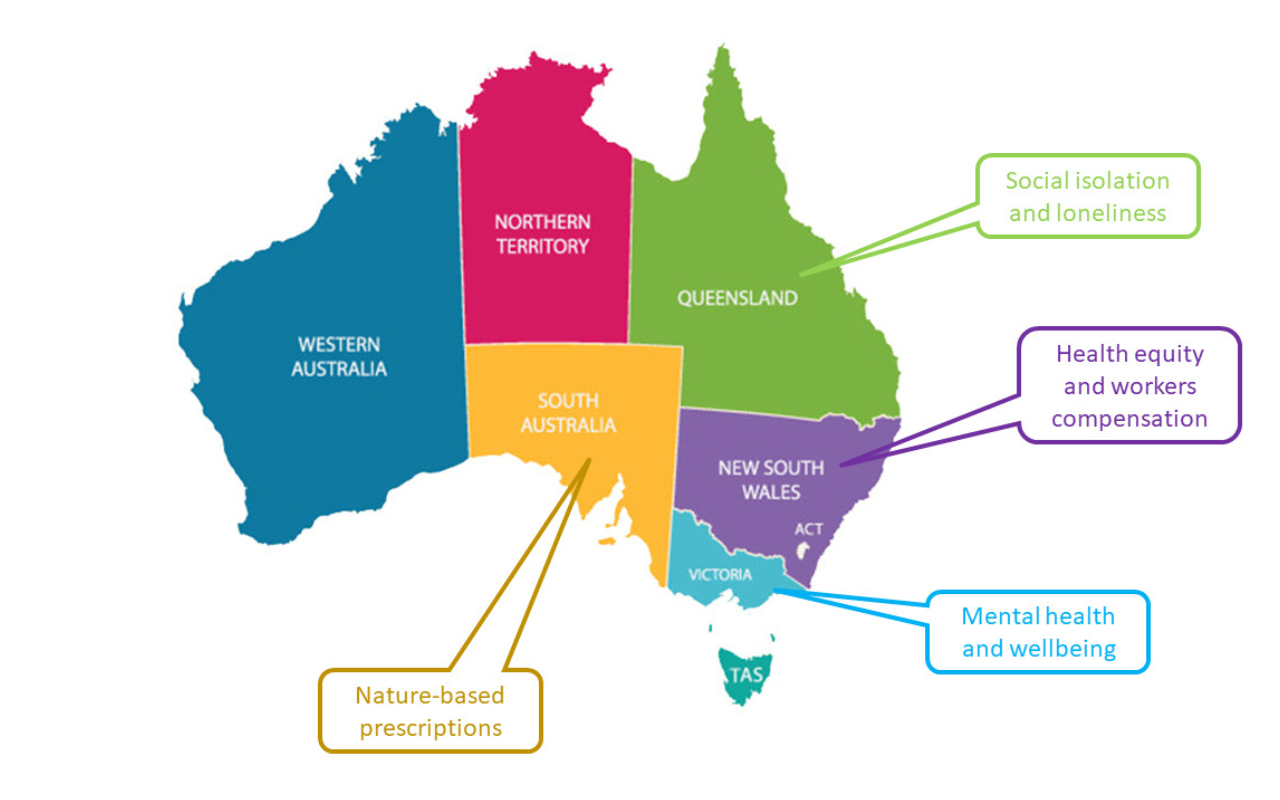
Holistic approaches to wellbeing have long existed, particularly in Aboriginal and Torres Strait Islander health care practices, which emphasise community, culture and connection to Country. Yet formal social prescribing approaches within the Australian health and social care sectors continue to evolve slowly from small, localised projects into a more significant element of the country’s health strategy. Embedded within frameworks like the 10-Year National Preventive Health Strategy and the Primary Health Care 10 Year Plan, the size and reach of social prescribing models have expanded under the leadership of primary health networks. Models have also been adapted across state and territory governments to address chronic disease, mental health and support for remote and vulnerable populations (Figure 1).
Over the past five years, two national roundtables have culminated in a consensus statement signed by over 100 leading health and consumer organisations, advocating for broader adoption of social prescribing and whole-of-system funding, with key organisations shown in Box 2.
| Royal Australian College of General Practitioners (RACGP): emphasising the central role of general practice in the rollout of social prescribing |
| Pharmaceutical Society of Australia (PSA): included social prescribing in its 2030 roadmap |
| Australian Social Prescribing Institute for Research and Education (ASPIRE): established in 2019, and plays a pivotal role in supporting national expansion of social prescribing and informing state and national policy |
| Consumer Health Forum: led a roundtable in collaboration with RACGP with a resulting report and recommendations |
| Australian Disease Management Association: a social prescribing hub and host a social prescribing community of practice |
| Australian Medical Students Association (AMSA) Social Prescribing Student Collective: an initiative group aiming to educate medical students about social prescribing. |
The how: medical and health care professional training
There is a growing need to formally incorporate prescriptions that address social needs in undergraduate and postgraduate medical and health education curricula to support health care professionals to effectively address the determinants contributing to health. There are no clear standards for education in social prescribing in Australia, although international training programs, especially from the UK, provide some guidance. Given the novelty of this field in Australian health care, training in social prescribing must not be limited to knowledge, but importantly to implementation and evaluation in diverse models of care, especially in primary care settings. Box 3 outlines key social prescribing education elements.
| Core principles and definitions |
| Impact of lifestyle and social determinants on health |
| Assessing social need |
| Community engagement |
| Asset mapping |
| Evidence-based practice in social prescribing |
| Collaborative approaches to interdisciplinary care and supervision |
| Culturally competent practice |
| Rural and remote adaptations |
| Technology use |
| Funding and sustainability |
| Implementation |
| Evaluation |
Some enterprising Australian universities, such as James Cook University, are beginning to explore ways to embed social prescribing education across undergraduate pre-clinical and clinical medical programs, as well as within lifestyle medicine curricula and emerging courses.
Medical students are embracing an expanding vision of health care that moves beyond the biomedical model toward person-centred, holistic care. The UK shows the driving role that students can play. The NHS social prescribing student champion scheme was established in 2015 with funding and support from NHS England. A small scale initiative, driven by student champions across UK-based medical schools, has expanded significantly over the past seven years; with social prescribing now embedded in the curricula of all 44 UK medical schools and taught in over 20 universities offering nursing, midwifery, and allied health care courses, including delivery of over 1500 peer-teaching sessions and establishment of #SocialPrescribingDay, a global awareness campaign reaching over 60 million people annually. This growth highlights the substantial role that student-led efforts have played in shaping medical education and promoting a holistic approach to health care. The social prescribing student champion scheme: 7 years on report offers further insights into the program’s success and provides a framework for global adaptation.
Next steps
Enabling integration of social health initiatives within the Australian health care system requires a number of significant changes, as outlined in Box 4.
| Formalised training programs across undergraduate and postgraduate health professional training |
| Expansion of national policy, structures and funding to support the scaling of social prescribing, including: – paid link worker/connector roles – support of social care sector – digital infrastructure (directories, assessment tools, service platforms) – Medicare integration of social care plans |
| National frameworks for quality and research: – clinical research funding streams – minimum dataset and evaluation framework |
| Greater integration and coordination of health and non-health services |
While significant changes are required to incorporate social connection initiatives like social prescribing, the benefits to individual and community health and wellbeing, including flow-on effects due to improved health and reduced health service use, provide a positive return on investment.
Conclusion
Understanding the social needs of patients and being aware of existing social prescribing options locally will help clinicians better support holistic wellbeing needs, and is an effective use of increasingly scarce resources. Formalised training for medical and other health care students is essential to equip future practitioners with the capability to meet the broader needs of the community. These opportunities will allow us as a society to be more proactive and create the infrastructure to address the SDH, alongside a more sustainable and equitable health care system.
Dr Rajna Ogrin works as a Senior Research Fellow at Bolton Clarke, Australia’s largest not-for-profit aged and community care provider. She is currently leading project that is codesigning, implementing and evaluating a social connection program, Connect Local , in metropolitan Melbourne.
Dr Sam Manger is a clinical and academic General Practitioner, Academic Lead of the Postgraduate Degrees in Lifestyle Medicine at James Cook University College of Medicine and Dentistry, Immediate Past-President of the Australasian Society of Lifestyle Medicine, Ambassador for the Federal Government initiative Equally Well Australia and host of The GP Show podcast.
Abbey Deguara is currently in her fifth year in her medical degree and was the lead of the Australian Medical Students Association Special Interest Group in Social Prescribing. She is passionate about mental health.
A/Prof JR Baker is an Australian leader in social prescribing, complex care coordination and link work services. JR is driven by his ideas on providing optimal health services through innovation in the not-for-profit, health space. He is the founder and Chair of the Australian Social Prescribing Institute of Research and Education.
Dr Bogdan Chiva Giurca works a British physician, currently working as the Clinical Lead and Global Director of the National Academy for Social Prescribing which was founded in 2019 by the Secretary of State for Health and Social Care. Bogdan has played a key role in the development of Social Prescribing in England since 2015 through establishing and chairing the NHS England Social Prescribing Champion Scheme (2015-2022) consisting of over 20,000 doctors, medical and healthcare trainees championing the subject in their own institution.
Prof Judy Lowthian is an Adjunct Professor with Monash University’s School of Public Health & Preventive Medicine and the University of Queensland’s Faculty of Health and Behavioural Sciences and Chair and Board Director of Maryborough District Health Service (Vic). Recent roles include 8+ years as Head of Research and Principal Research Fellow at Bolton Clarke, Steering Committee member of ROSA (Registry for Senior Australians), Advisory Board member of Ending Loneliness Together, and Adjunct Professor with The University of Queensland’s Faculty of Health and Behavioural Sciences.
The statements or opinions expressed in this article reflect the views of the authors and do not necessarily represent the official policy of the AMA, the MJA or InSight+ unless so stated.
Subscribe to the free InSight+ weekly newsletter here. It is available to all readers, not just registered medical practitioners.
If you would like to submit an article for consideration, send a Word version to mjainsight-editor@ampco.com.au.

 more_vert
more_vert
Big advocate for this. I recall as a student in outback Qld in 2003 a distressed mother who had trouble doing things for herself was given a script by the RFDS
doctor visiting her small town:
‘Read Harry Potter 2-3 times weekly until finished’!!
Terrific article, thanks!