InSight+ spoke with Monash University researchers about a new breakthrough they say could revolutionise immunotherapy for cancer.
A study from researchers at Monash University (Australia) and Southampton University (UK) has described a previously unknown function of cell protein that may lead to a vaccine for multiple types of cancer.
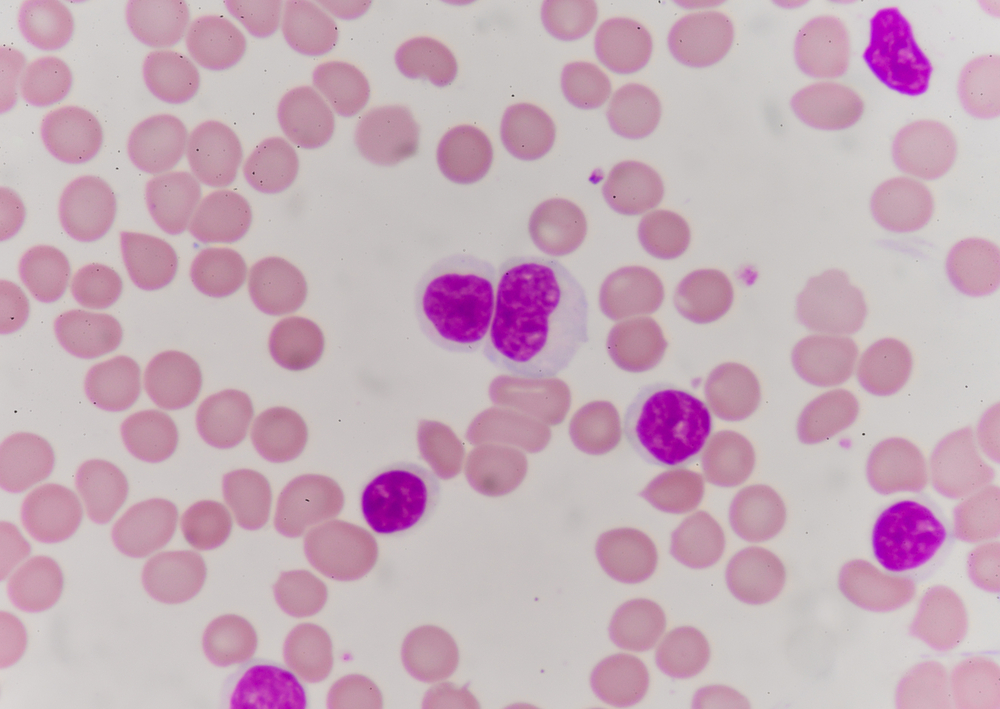
The researchers found that the XPO1 protein — which is associated with the growth of cancerous cells — produces a peptide that attracts immune system natural killer (NK) cells.
The researchers also found that cancer patients with higher levels of XPO1 had increased longevity associated with the infiltration of the tumor by NK cells.
Professor Anthony Purcell is a professor (research) in biochemistry and molecular biology at the Monash Biomedicine Discovery Institute.
“So, there’s this new player. We’ve known about natural killer (NK) cells in the context of cancer previously, but never in this specific modality (of cancer recognition). And we were able to map NK cell infiltration of XPO1 expressing tumour, and link it to patient survival,” said Professor Purcell.
“It’s indirect evidence, but it’s strong and pretty striking,” he said.
An outside-the-box idea
Professor Purcell said the idea originated around ten years ago, when he and lead author hepatologist Professor Salim Khakoo worked together at Southampton University.
“Our expertise at Monash University is in the antigen discovery component, and we’re quite well known internationally for doing this type of work. The team at Southampton has the cancer, and NK cell, expertise,” said Professor Purcell.
“We came up with the idea to look at a human leukocyte antigen [HLA] molecule called HLA-C, which is one of three types of HLA on the surface of our cells, including cancer cells,” Professor Purcell told InSight+.
“[Professor Khakoo] had an interest in natural killer cells, and particularly in killer inhibitory receptors (KIR). One KIR in particular — KIR2DS2 — activates the natural killer cells (NK). These NK cells are part of the innate immune system,” said Professor Purcell.
“One of the roles of [HLA-C] is to display fragments of cancer proteins on the cell surface to alert immune cells that there’s something wrong with the cell. In this case, however, we found that the KIR2DS2 molecule was actually recognising HLA-C in the context of quite a specific [antigen], called XPO1,” he said.
“The XPO1 protein has had a link to several types of cancer including haematological malignancy (blood cancer). The breakthrough is that this innate cell can specifically recognise a cancer antigen, XPO1 bound to HLA-C molecules. It is adaptive-like in its recognition,” said Professor Purcell.
“A hallmark of adaptive immunity is its capacity to generate immune memory, which is important if the cancer comes back, or if there is metastatic growth,” said Professor Purcell.
“Immune memory is the goal of vaccination,” he said.
Increased patient longevity
The study combined biochemical research with data from the TCGA Cancer Genome Atlas, a large genomic repository hosted at the National Cancer Institute in the United States.
“We married [our research] to a retrospective study where we’re able to show that expression of this antigen and infiltration of the tumour by NK cells is associated very strongly with patient survival in a number of different cancers,” said Professor Purcell.
“If we look in patient survival, those that have NK cells plus expression of this XPO1 antigen, do a lot better. There’s significant circumstantial evidence that this is the case,” said Professor Purcell.
More options for cancer vaccination
The team is hoping to create the world’s first cancer vaccine using natural killer cells.
“There are a number of vaccines and trials at the moment in the context of cancer,” said Professor Purcell.
“The difficulty is finding which target, or which protein should be used in the vaccine.”
“There’s always a risk that, if it’s a protein that’s also found in the heart, for example, you could induce inflammation in the heart and obviously cause problems. The idea around XPO1 and this axis is that there’s potential to direct the NK cells to the tumour, as well as potentially other types of immune cells such as T cells,” said Professor Purcell.
Professor Purcell explained that these killer cells could be educated to attack tumours in a new way.
“So currently we know how to direct killer T cells — which are another type of killer cell — toward a tumour, either through vaccination or immunotherapy. Immunotherapy using ‘checkpoint inhibitors’ target T cells to essentially turn the brake off them and help them enter the tumour, and potentially recognise antigens from the tumour,” said Professor Purcell.
“We’re adding a new player to the process by educating the NK cells through recognition of a cancer antigen, allowing a double-barrelled approach to try and eliminate the tumour.”
The researchers hope that these new data will lead to more personalised cancer vaccines.
“It’s just a smarter way to vaccinate or treat. The sooner you can predict with confidence the best treatment, you can hopefully make a difference to the patient.”
Subscribe to the free InSight+ weekly newsletter here. It is available to all readers, not just registered medical practitioners.

 more_vert
more_vert