The National Lung Cancer Screening Program will begin in July 2025, with the hope that it will save lives by detecting cancer at an earlier and more treatable stage.
Although lung cancer isn’t Australia’s most common cancer, it’s the deadliest. It kills more men and women than any other cancer. People don’t tend to be diagnosed until the later stages, when symptoms such as a cough appear. Sadly, the later the diagnosis, the poorer the survival rate. Screening will save lives by detecting cancer at an earlier and more treatable stage. It will reduce the number of patients needing treatment for advanced stage lung cancer where the survival rate is much lower.
The National Lung Cancer Screening Program (NLCSP) will begin in July 2025 and will operate similarly to other early detection programs, such as the national bowel cancer and cervical cancer screening programs. Participation in national screening programs for breast, colorectal and cervical cancer has been associated with substantially better outcomes — higher probability of survival and lower death rates. The cervical cancer death rates have halved since its screening program was introduced in 1991.
Lung cancer is the most common cancer diagnosis for Aboriginal and Torres Strait Islander people. The NLCSP is working in partnership with the National Aboriginal Community Controlled Health Organisation to make sure the screening program is culturally safe, equitable and accessible for Indigenous peoples.
The program is targeted at people aged between 50 and 70 and who have no signs of lung cancer, have a history of smoking and are still smoking or have stopped in the last 10 years.
The NLCSP will use low-dose computed tomography (LDCT) scans to look for lung cancer. The Health Minister Mark Butler announced the program in May 2023 – allocating $264 million for the program that has the potential to save 12 000 lives in the first decade of the program.
The program pathway
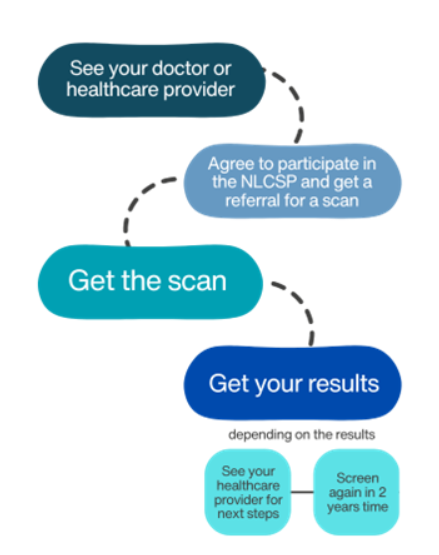
Source: https://www.health.gov.au/our-work/nlcsp/how-it-works
At-risk Australians will be eligible to have the scan every two years while they participate in the program or until a lesion is found and needs to be treated. People who have a low or moderate risk of lung cancer will be screened again in 3 or 12 months and may be referred to a specialist. High-risk patients will be referred to a specialist and linked with a multidisciplinary team.
If the screening results find something that needs to be followed up, the patient will be referred back to their health care provider for the next steps.
Clinicians, peak bodies, and consumer organisations worked with the Department of Health and Aged Care (DHAC) on the design and implementation of the NLCSP.
Guidelines are being developed to manage the patients’ journey with the NLSCP.
The DHAC said the guidelines will include:
- steps of the screening and assessment pathway, including participant recruitment and eligibility;
- information on providing smoking cessation advice and support;
- the requirements for shared decision-making;
- LDCT scan referral, screening, and assessment;
- recommendations and practice points;
- links to existing diagnostic and management pathways, and guidelines, related to suspected lung cancer and for incidental findings.
There will be two new Medicare Benefits Schedule (MBS) items for the LDCT scans, one for the two-yearly scan and for scans needed for any follow up. Radiology providers will be required to bulk bill the scans when using the NLCSP related MBS items.
Radiologists will be required to report NLCSP screening information to the National Cancer Screening Register, similar to the bowel and cervical screening programs.
Subscribe to the free InSight+ weekly newsletter here. It is available to all readers, not just registered medical practitioners.

 more_vert
more_vert