For the second time in three years, mpox has been declared a global health emergency — the highest level of alert given by the World Health Organization (WHO). Such a declaration demands continued monitoring, surveillance and response to ameliorate further transmission.
This year, mpox spread quickly in central and western Africa, especially in the Democratic Republic of Congo (DRC), where the virus is endemic, and has spread to the nearby countries of Rwanda, Kenya, Burundi and Uganda. A new more dangerous strain has emerged, clade Ib, and single clade Ib, with cases confirmed in both Sweden and Thailand.
In 2022–2023, a global outbreak of mpox was caused by the less virulent clade II strains, now also resurging globally, with 106 310 cases and 234 deaths in 123 countries. In 2024, to August 31, cases surged by 28% in the African region, 89% in the European region and 68% in the western Pacific region.
In Australia, the clade Ib virus has not yet been reported, but a surge of mpox cases (clade II strains) has occurred since August. In 2024, 606 cases have been reported, with a total of 774 total cases to date. Recent data from Queensland notes that there have been 51 confirmed cases of clade IIb mpox notified in 2024. There have been no deaths reported due to mpox in Australia.
What is mpox?
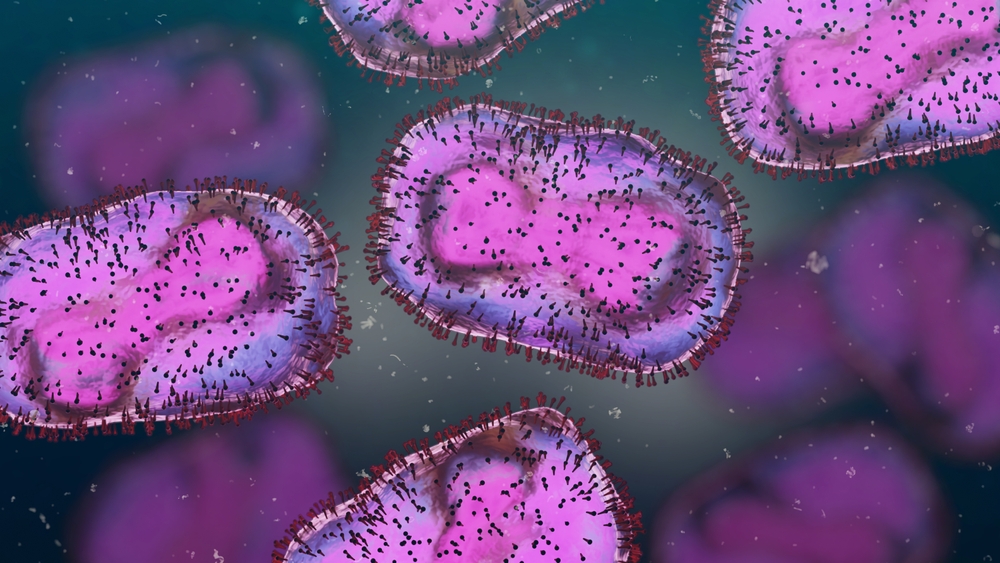
Mpox is a double-stranded DNA virus closely related to smallpox, belonging to the genus Orthopoxvirus within the Poxviridae family. Two clades exist; clade I, which has a higher mortality rate, with subclades Ia and Ib, and clade II, with subclades IIa and IIb. Mpox is a zoonotic disease and until recently was generally confined to several African countries where it is endemic and has been circulating for decades. Various animals carry the virus, including squirrels, Gambian pouched rats, dormice, and various species of monkeys.
Genome sequences of the mpox clade Ib virus are publicly available on the GISAID database where the phylodynamics and the latest variants are also monitored. Sequence comparison of 14 poxvirus surface antigen proteins suggests that clade Ib did not show major differences from the current vaccine strain, suggesting that current vaccines will still offer good protection (~85% efficacy).
How is mpox spread?
In the 2022 global outbreaks, mpox was predominantly spread by sexual contact. This was the first time mpox became a sexually transmitted disease, predominantly by men who have sex with men (MSM). The newer clade Ib strain is also spread by sexual contact, skin-to-skin interactions, respiratory droplets and body fluids. Contact with infected animals, contaminated surfaces, objects or fabrics (like bedding and clothes) are also common means of transmission. The virus may be passed on in the asymptomatic phase (1 to 4 days) and during the symptomatic phase, until the rash has fully healed.
Epidemiological observations suggest that airborne transmission is not a primary mode of spread. The virus can also cross the placenta; however, vertical transmission has not yet been observed; in 2022, at least 12 pregnant women were infected but vertical transmission was not observed.
What are the symptoms of mpox?
Symptoms are similar to smallpox but less severe and commonly include a fever, an extensive characteristic rash, and swollen lymph nodes. The febrile stage lasts from 1 to 3 days. Further symptoms may include intense headache, back pain, myalgia and lethargy. After the initial febrile viraemic phase, the virus can spread to the tonsils, spleen and liver, which results in a second viraemia, enabling the virus to spread to the lungs, kidneys and intestines. The skin erupts with characteristic lesions, which develop from macules to papules to vesicles, followed by scabs over a 2- to 4-week period. The incubation period of mpox ranges from 5 to 21 days but may be unusually short with a 24-hour incubation period following sexual contact. It is important to distinguish mpox from other illnesses such as chickenpox/shingles, measles, bacterial skin infections, scabies, syphilis, gonorrhoea, chlamydia and medication-associated allergies. Chickenpox is frequently misdiagnosed as mpox where both are endemic.
Who is affected?
Groups most at risk are MSM, people living with HIV, health care workers and travellers. Those living with HIV and other immunocompromised or underlying conditions, as well as those with sexually transmitted diseases, are at increased risk of severe mpox disease and are more likely to be hospitalised.
The history of mpox
Before 1970, there were no documented cases of human mpox but it was known as an infection in monkeys and apes. The first human mpox case was reported in 1970 in the DRC and the virus is now endemic in Benin, Cameroon, the Central African Republic, the DRC, Gabon, Ivory Coast, Liberia, Nigeria, the Republic of the Congo, Sierra Leone, and South Sudan.
Surveillance data between 1970 and 2015 in Africa showed that mpox occurred mainly in children under 10 years, with an increasing number of cases over time as the population became more susceptible to mpox due to termination of mass smallpox vaccination. In the 2017–2018 outbreak in Nigeria, the average age affected was 29 years of age with 64% being male, but in the 2022 outbreaks affecting countries outside of Africa, males accounted for 96.8% of the cases, and the median age was 34 years.
Case fatality rate (CFR) estimates have varied over time and for clade II are reported as 3.6% and for clade I as 10.6%; however, the 2022 outbreaks have an estimated overall CFR of 0.08%, most likely due to active surveillance, and a rapid response involving early diagnosis and treatment.
The reproduction number (R0) has also changed over time. Surveillance from 1980 to 1984 estimated R0 to be 0.8, but early estimations of the R0 in the 2022 outbreak in non-endemic countries ranged from 1.54 in Belgium to 3.62 in Germany, supported by similar studies around the globe, suggesting sustained human-to-human transmission, predominantly due to social and/or sexual behaviours; however, because of education, changes in behaviours, hygiene awareness, infection-induced immunity, early diagnosis and treatment, and vaccinations in susceptible populations, transmission virtually came to a halt, allowing the WHO to rescind its PHEIC declaration in 2023.
Vaccines
There are no specific vaccines for mpox, but due to shared antigenic features, the smallpox vaccines give ~85% cross-immunity against mpox. There are three vaccines available for use: ACAM2000, JYNNEOS and LC16m8.
ACAM2000 was licensed in 2007 by the US Food and Drug Administration (FDA) for the prevention of smallpox, and mpox post-exposure prophylaxis; however, vaccine safety is still of concern as cardiac complications and painful cutaneous reactions may result. Vaccinia immunoglobulin (VIG) is preferred for the treatment of complications associated with ACAM2000.
Modified vaccinia virus Ankara Bavarian Nordic (MVA-BN) vaccine, JYNNEOS, was licensed by the FDA in 2019 for prevention of mpox in adults aged over 18 years. It is considered safer than ACAM2000; however, both have been recommended for mpox high-risk groups.
LC16m8 is only licensed in Japan, is a third-generation attenuated vaccine, and has been shown to be protective against mpox in animal models.
Vaccines in Australia
In Australia, ACAM2000 is licensed but JYNNEOS is not; however, JYNNEOS has been made available via a special emergency pathway under section 18A of the Therapeutic Goods Act 1989 and is indicated for use in those 16 years and older. Both vaccines are available in Australia and JYNNEOS is preferred but there are limited international supplies. For this reason, the following are generally prioritised: close physical contacts of people infected with mpox; MSM groups; immunocompromised individuals; and those in occupations with increased exposure to mpox, including sex workers, laboratory staff and health care workers. For anyone in these risk categories planning travel to a country experiencing outbreaks, vaccination is recommended 4 to 6 weeks prior to departure.
JYNNEOS is a 2-dose vaccine; the second dose should be given 4 weeks after the first dose. The Australian Technical Advisory Group on Immunisation (ATAGI) does not recommend booster doses of the mpox vaccine for people fully vaccinated, or recovered from an mpox infection, including those who are severely immunocompromised. Some studies suggest that vaccine-induced immunity begins to wane at around 3 to 4 months post-vaccination, dropping close to baseline by 10 to 24 months.
Antivirals used for mpox
There are no approved antivirals to treat mpox, but antivirals like tecovirimat, which were originally developed for smallpox, have shown efficacy in treating severe cases. For most immunocompetent patients, supportive care and pain control is sufficient. Some patients will suffer severe manifestations including: ocular infections, myopericarditis, neurologic complications, and complications associated with oral, rectal, genital, and urethral mucosa. Uncontrolled viral spread may affect immunocompromised patients and those with severe skin conditions.
Tecovirimat, brincidofovir, and cidofovir have been studied. Tecovirimat, a 4-trifluoromethylphenol derivative, was approved by the US FDA in 2018 and the European Medicines Agency in January 2022 for the treatment of smallpox and cowpox. For mpox, safety studies are positive but efficacy is marginal against clade I; however, in a recent study, mortality was shown to be markedly reduced. It has been recommended to be administered as first line for mpox treatment especially in pregnant and breastfeeding patients.
Cidofovir (CDV or Vistide) is an acyclic nucleoside phosphate that was approved by the FDA in 1996 for the treatment of cytomegalovirus retinitis in HIV patients and may prove useful against mpox. Brincidofovir (CMX001 or hexadecyloxypropyl-cidofovir), a CDV derivative, was approved for smallpox treatment in 2021 by FDA, and is less toxic than CDV but further evaluation in human mpox treatment is needed. These drugs can be considered if tecovirimat is contraindicated or they can be used in addition to tecovirimat in serious cases.
Trifluridine is an ophthalmic antiviral drug that has been shown to inhibit replication of several viruses, including vaccinia virus, and could also be considered for mpox in severe cases.
Prevention and control
Vaccination and antiviral drugs are important tools to prevent and control mpox but alone are unlikely to halt the march of the virus around the world. Surveillance in endemic regions, and rapid identification and isolation of new cases until recovery, is critical, as is education by raising awareness of risk factors, and the measures people can take to reduce exposure. Simple measures include: avoiding close contact with infected individuals or animals; good hygiene practices; getting vaccinated if at high risk or exposed to the virus; and the use of personal protective equipment in health care settings. People who are vaccinated, or recovered, should also continue to reduce exposure to mpox as reinfection is possible but symptoms are milder.
Mpox has emerged and re-emerged for over five decades and knowledge of the factors that modulate animal-to-animal transmission and spill-over to humans is limited; moreover, we are not closer to reliable prognostication of virus emergence.
Importantly, vaccines, antivirals and diagnostic capacity are not readily available to low and middle-income countries and an unknown number of mpox cases in these countries are not detected due to limited surveillance capacity.
Mpox is a highly contagious virus and as a global community, we must be on high alert. The new emerging clade Ib virus is more infectious and severe than the previous clade strains circulating in Africa over previous decades and presents an epidemic and pandemic threat.
Gary Grohmann is a former director of immunobiology at the Therapeutic Goods Administration. He currently works as an independent consultant virologist. He is a board member and member of the scientific advisory committee of the Immunisation Coalition and an adjunct professor at the University of Sydney.
Acknowledgement: Gratitude to Professor Robert Booy for reviewing the manuscript.
The statements or opinions expressed in this article reflect the views of the authors and do not necessarily represent the official policy of the AMA, the MJA or InSight+ unless so stated.
Subscribe to the free InSight+ weekly newsletter here. It is available to all readers, not just registered medical practitioners.
If you would like to submit an article for consideration, send a Word version to mjainsight-editor@ampco.com.au.

 more_vert
more_vert