As we mark the 40th anniversary of Medicare, Australians are long overdue a clear discussion about how we can guarantee funding for GP services into the future.
2024 marks the 40th year of Australia’s Medicare, and it has been fitting that a number of initiatives have marked the milestone. Some ideas were good, while others — such as a commemorative Medicare card — were perhaps a little passé. Overall, the anniversary has provided the opportunity for serious consideration and reflection on the achievements of this program that brought universal health coverage to all Australians. The year has provided an opportunity to step back, consider the current state of Medicare, and to sense-check its suitability for the future.
We have attended a number of these events, and one of us (MW) has had the opportunity to present at a recent Canberra event. Many of the speakers approached Medicare from the perspective of economics, governance or social significance. As the sole GP invited to speak, it was an important chance to highlight the intense pressures that general practice faces due to chronic underfunding of GP services within Medicare.
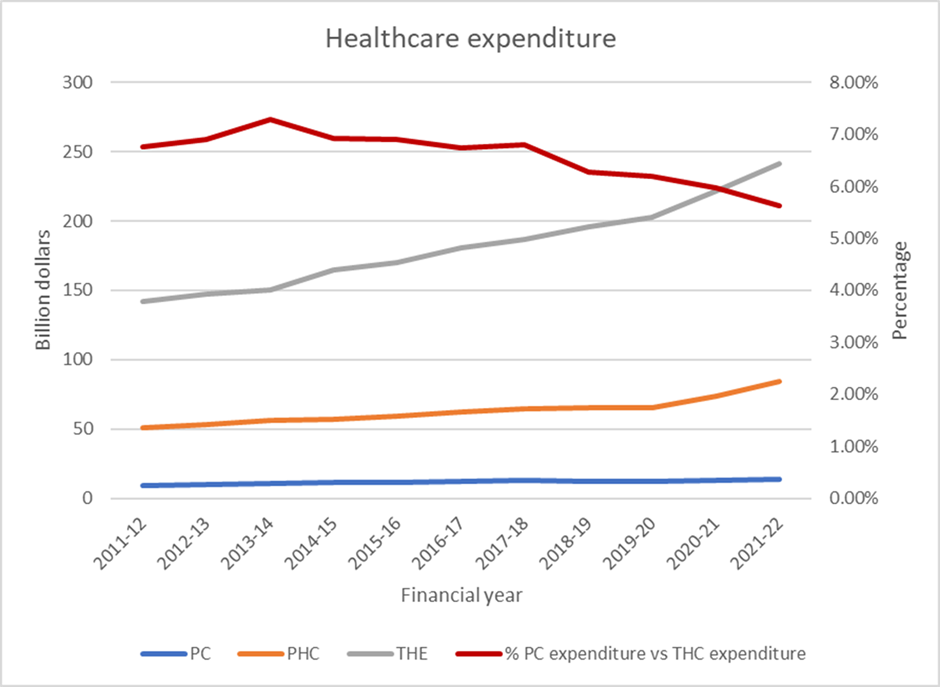
Figures were presented at the Canberra forum showing changes in health expenditure in Australia over the last decade. The data revealed that total health expenditure has grown by $100 billion per year and sits at $240 billion in the most recent figures from 2012–22. This is deceptive, however, as unadjusted expenditure figures do not consider inflation — $100 billion in 2012 had the same buying power as $126 billion in 2022 — so we must temper our understanding of the figures.

The data showed that around 40% of health expenditure goes to hospitals, and hospital expenditure accounts for most of the cost increases over the last decade. This compares with Medicare spending for primary care services provided by GPs, which at one point represented more than 7% of health expenditure and has barely increased over the last decade. Worryingly, funding for this part of the health system, which provides the majority of Australia’s primary care services, has been dropping as a percentage of health expenditure for most of the last decade and has dropped to less than 5.7% in the 2021–22 figures.
A different way of looking at this drop comes from the most recent Review of Government Services Report from the Productivity Commission, which showed that per person funding for GP services dropped by around 8% in the 2021–22 financial year, having also dropped by a small amount in the previous year. This represents around a billion dollars of funding for comprehensive high quality primary care services that has been stripped from patient rebates in the last year. To put all of this in perspective, the increases in hospital expenditure — not the total spend on hospital but the additional amount of expenditure — is approaching the total amount spent on GP services. This is an extraordinary fact that we have not seen highlighted.
It is obvious to all — patients, politicians, and practitioners — that the viability of general practice as we have known it is weakening rapidly. Many clinics that had held out through the long financial winter of the Medicare indexation freezes are now introducing, or increasing, out-of-pocket fees as a mechanism for recovering costs no longer met by Medicare rebates, even with the additional bulk-billing incentives designed to bandaid the losses. These out-of-pocket costs have enormous potential to impact patient’s ability or willingness to attend their GP: around the country, doctors are telling me that consultations are more complex as patients, understandably, want to get their money’s worth.
Australia has a ten-year Primary Healthcare Plan and a report from the Strengthening Medicare Taskforce, both of which highlight the formidable challenge of making primary care accessible and affordable for all Australians. The reduction in GP funding makes that challenge of providing accessible and affordable primary care for everyone who needs it, increasingly difficult.
Australians are long overdue a clear discussion about how we can guarantee funding for GP services and allow Australians to retain access to comprehensive coordinated high quality primary health care. Such health care has been a feature of Medicare over the last 40 years and has been one of the major contributors to making Australia a healthy nation with world leading health care outcomes, and yet modest health expenditure as a proportion of gross domestic product compared to the UK, New Zealand, Canada, and USA. There is now great urgency in returning adequate funding to general practices whether through increased Medicare Benefits Schedule rebates or other funding models.
The past two decades have seen multiple experiments looking at changing GP funding, whether it be from coordinated care trials back in the 1990s, the Diabetes Care and the Health Care Homes trials. All of those trials showed that care can be improved by investing more in GP services but that this did not lead to cost savings in the short term.
Policy makers and bureaucrats continue to talk about different funding models for primary care and “focusing on better value”. Few have ever treated a patient themselves or run a general practice. International evidence has shown that systems that focus on supporting access to high quality primary care services provide best value for money. Perhaps it is less about the funding model and simply more about the funding.
Nobody should be surprised that GP clinics are struggling with increasing concerns about viability, that we hear established practices are more likely to merge, and that fewer and fewer medical students are choosing a career in general practice. Should those trends surprise us when, despite the breadth and joy of a general practice career, doctors see an immediate loss of entitlements and a drop in income when they consider leaving the hospital sector?
The purpose of this article is to highlight this issue, so fundamental to health care in Australia, and to stress the urgent action needed to better support GP training and the transition from medical students to community specialist general practitioner. It is way past time that we start setting some benchmarks for how much of the health budget is spent on GP services.
Hopefully we are not already too late…
Dr Michael Wright is a GP, health economist and health services researcher in Sydney, and the Chief Medical Officer of Avant Mutual.
Steve Robson is an obstetrician, gynaecologist, and health economist. He is president of the AMA.
The statements or opinions expressed in this article reflect the views of the authors and do not necessarily represent the official policy of the AMA, the MJA or InSight+ unless so stated.
Subscribe to the free InSight+ weekly newsletter here. It is available to all readers, not just registered medical practitioners.
If you would like to submit an article for consideration, send a Word version to mjainsight-editor@ampco.com.au.

 more_vert
more_vert
The article provides a crucial wake-up call about the future of Medicare and the sustainability of GP services in Australia. While the challenges are significant, they are not insurmountable. By adopting a multifaceted approach that includes increasing funding, implementing value-based care models, investing in workforce development, enhancing integration, and engaging patients, we can secure the future of general practice and ensure that Medicare continues to provide high-quality, accessible healthcare for all Australians.
Some Potential Resolutions
Increase Medicare Rebates: To address the immediate financial strain on GPs, increasing Medicare Benefits Schedule (MBS) rebates is essential. This would help cover the rising costs of providing high-quality primary care and reduce the need for out-of-pocket expenses for patients.
Implement Value-Based Care Models: Transitioning to value-based care models that reward quality and outcomes rather than volume of services can help ensure that funding is directed towards effective and efficient care. Pilot programs and phased implementation can help identify best practices and potential pitfalls.
Invest appropriately in GP Training and Workforce Development: Strengthening support for GP training programs and providing incentives for medical students to pursue careers in general practice can help address workforce shortages. This includes offering scholarships, loan forgiveness programs, and competitive salaries to attract and retain talent in primary care.
Enhance Integration and Collaboration: Promoting better integration and collaboration between primary care and other healthcare sectors, such as hospitals and community services, can improve patient outcomes and reduce duplication of services. This requires investment in health information technology and shared care models.
Engage Patients and Communities: Actively involving patients and communities in discussions about the future of Medicare and GP services can help ensure that reforms meet the needs and preferences of the population. This can be achieved through public consultations, patient advisory panels, and community health initiatives.
Sobering figures, for sure, but no surprise to most of us – any of us actually. I have long maintained that as the funding increase needed to reposition GP in its rightful place is so significant, this uplift is unlikely to come in the form of realistically increased rebates under the fee for service model. That being so, the move to the single employer model being trialled in several places for the registrars might well provide an example of the direction that GP funding might take for all GPs who desire a salaried option with associated entitlements such as those other public servants enjoy. I’m retired now, but when I think of the amount of just long service leave I would have accrued, it makes me feel a bit sick. No wonder the registrars have woken up to the unfair impact the present system offers once they enter general practice.
General practice is the backbone of our excellent health system. Without it functioning well throughout Australia, the health of every person will eventually suffer. There will be inadequate care for chronic disease, inability to see a GP urgently, and extreme pressure on both public and private hospital care. It needs to be funded at a reasonable level, recognised as a speciality, to maintain the existing practices and to encourage new graduates to enter one of the most rewarding areas of medicine.
Great article Michael. We are a small bulk billing practice situated 1.5 km from GCUH and literally we are battling to make ends meet due to all the factors you have discussed. Now a satellite rapid access service is planned for Southport! We are up to our eyeballs in debt and I just don’t think we can hang on without practice nurses, etc. I don’t want to give up the practice as I have lived 25 years and call Australia home. We need more spent on us as GP’s -period
Agree with Chris Mitchell – thank you both. Evidence based is the way to advocate for change so good to see this shift away from rhetoric.
Yes great summary. Universal access to high quality primary care is the cornerstone. The figures demonstrate that fixing investment in general practice is well within our means. Investing just the annual increase in hospital spending would double GP spending. Can we please have action before it is too late.
Great article Michael Wright and Steve Robson thanks