As our population ages, we must ensure our health and aged-care systems are able to deliver appropriate care to a growing number of people with dementia, especially in rural and remote Australia.
As life expectancy continues to increase, Australian society is ageing. With increasing age, the prevalence of dementia goes up, and the health and aged-care systems need to adapt to this. The Royal Commission into Aged Care Quality and Safety (2021) exposed many failings in the delivery of aged-care services to older Australians and specifically identified that “the quality of dementia care in the aged care system needs significant and immediate improvement”. Unsurprisingly, the Commission revealed that care in rural and remote areas, where workforce challenges are well described, needed particular attention in terms of improving care outcomes.
A well trained and caring workforce with specific understanding of the needs of older people was identified as an area needing attention. It is important that people are treated with respect and receive care that maintains their dignity as they age. As people become frailer, more infirm and have limited capacities and freedoms, they become vulnerable. Older people with cognitive impairment or dementia are recognised as particularly vulnerable and require better approaches to care, whether they are living at home with support or in a supervised environment such as residential aged care.

Several non-government organisations, such as Dementia Australia and Dementia Training Australia (DTA), have expertise in this field and are tasked with improving community understanding of dementia, supporting carers and those affected by dementia and upskilling health professionals in dementia care. Although these areas have had ongoing attention and support over many years, the uptake of available training has often been suboptimal. Specific consideration of the needs of rural and remote providers has received limited attention so consideration of their needs is warranted. After all, improvement approaches are critically dependent on context, so understanding what works, for whom and under what circumstances is essential to maximising the benefit from the resources available and to development of future initiatives.
In 2023 we undertook a review focused on training for the aged-care workforce in rural and remote areas, a collaboration with DTA. This presented an opportunity for dedicated effort to learn more about the experiences, views and training needs of aged-care service providers working in rural and remote Australia. We started by looking at the published literature to see what was already described. Our search focus was narrow, specifically exploring the barriers and enablers in training rural and remote providers around dementia. Findings from the review are to be used in a co-designed process aiming to develop a framework to enhance development and delivery of DTA training to the rural and remote dementia health care workforce.
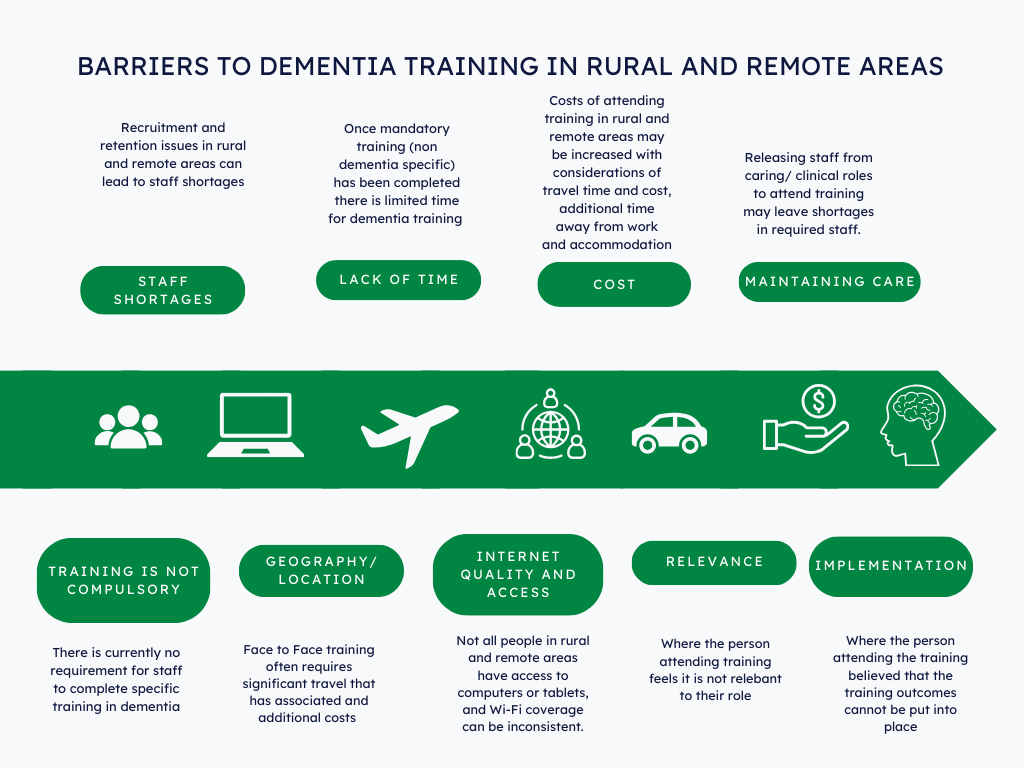
After searching relevant bibliographic databases, including national and international grey literature and government reports, we found limited literature on the issues for rural and remote aged-care providers, all from Australia or Canada. The most common barrier preventing rural and remote health professionals accessing dementia training was the low staffing levels. Staff were unable to take time away from caring for patients to undertake education or training. Other barriers included limited access to a high-speed, high quality internet connection, and limited training opportunities, funding and resources devoted to staff training. The lack of a mandatory requirement for training in dementia in a landscape where many other training programs are mandatory, has meant that professional development opportunities around dementia management have not been prioritised. Rural and remote providers also face challenges around distance from metropolitan areas, with increases in time and travel expense, which limits providers or training providers travelling. Given the small workforce in rural and remote areas, face-to-face training was reported as being cost prohibitive for training providers.
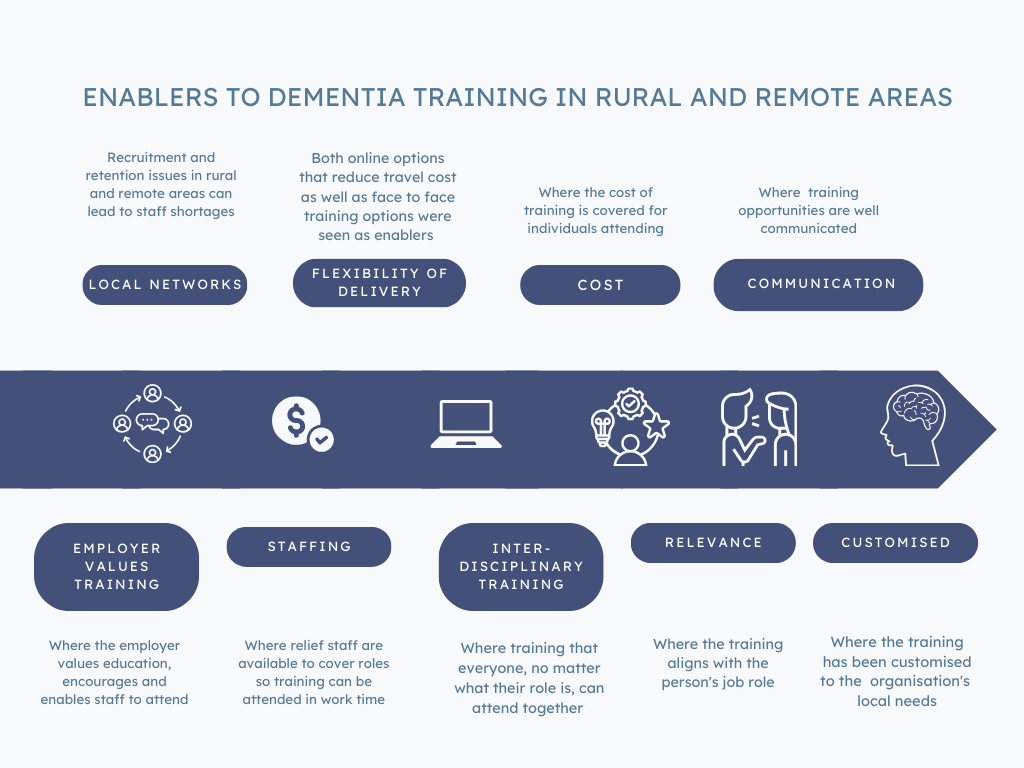
Enablers to participation in dementia training were online administration of training programs, as well as training providers collaborating with end users of the training to ensure it met the learning needs of the users. Matching educational needs to the job role, employer encouragement to complete training, paid time off work to attend training and the availability of relief staff were all important enablers. Other enablers of training uptake were offering training programs locally, alignment of organisational culture/values to staff training, regular communication between management and staff regarding training and a multidisciplinary approach to training.
Descriptions of successful approaches to dementia training were identified. Promising approaches included use of a “knowledge broker” embedded in residential aged-care facilities to facilitate knowledge translation strategies, and telehealth case conferencing on managing challenging patients with a metropolitan expert aged-care psychiatry consultation service. An Australian project used tele-mentoring, supporting clinicians to access collaborative learning in a knowledge-sharing network model (similar to a Community of Practice). There was a surprising gap in the literature related to best practice training for Indigenous peoples.
The published evidence on barriers and enablers specific to rural and remote health care professionals in accessing dementia training needs to be developed through direct workforce consultation. The analysis and reporting of our research project are being finalised. The findings will help refine strategies to ensure future resources and efforts are directed towards the appropriate delivery and content of the training that is urgently needed for upskilling the Australian rural and remote health workforce in dementia care.
This review was reported in greater depth in the Australian Journal of Rural Health (Thompson S, Shukralla H, Fyfe K, Newman E, Fitzgerald K. Barriers and enablers of dementia training in health care workers in rural and remote Australia: a scoping review to inform future approaches to training. Aust J Rural Health 2024 Feb 26.)
Sandra Thompson is the Director of the Western Australian Centre for Rural Health (WACRH), Chair of Rural Health at University of Western Australia and a professor of rural, remote and regional health. She is a public health physician with experience in science, health policy and management. Professor Thompson has vast research and evaluation expertise with interests including rural and Aboriginal health, prevention and management of chronic diseases, strengthening primary health care, and the attraction/retention of health professionals in rural areas.
Heidi Shukralla is a medical practitioner who undertook specialist training in public health medicine with the WACRH. Heidi has an interest in public health, rural and remote health, and Aboriginal and Torres Strait Islander health.
Katrina Fyfe is a senior research officer at the WACRH and previous state manager of Dementia Training Australia (WA/SA).
John Woods is a medically qualified health researcher at the WACRH.
Kathryn Fitzgerald is a rural allied health clinician and academic at the WACRH.
The statements or opinions expressed in this article reflect the views of the authors and do not necessarily represent the official policy of the AMA, the MJA or InSight+ unless so stated.
Subscribe to the free InSight+ weekly newsletter here. It is available to all readers, not just registered medical practitioners.
If you would like to submit an article for consideration, send a Word version to mjainsight-editor@ampco.com.au.

 more_vert
more_vert