The Australian and New Zealand Hip Fracture Registry is a clinical quality registry whose primary objective is to use data to drive change and improve outcomes for older people with a hip fracture.
In Australia, there are 19 000 hip fractures each year with total annual costs exceeding $1.01 billion. The costs associated with hip fracture are not merely monetary. Twenty-five per cent of people die within one year of hip fracture, many do not regain their function, and 11% of cognitively healthy and 46% of cognitively impaired people transition from home to residential aged care facilities (here).
The individual, community and health costs of hip fractures highlight the need to consistently provide effective and cost-efficient care aimed at facilitating recovery and preventing future fractures (here). To this end, the Australian and New Zealand Hip Fracture Registry (ANZHFR) was set up, informed by similar work in the United Kingdom, the Australian and New Zealand guideline for hip fracture care, and the Australian Commission on Safety and Quality in Health Care (ACSQHC) Hip Fracture Clinical Care Standard (2016 and 2023) (Figure 1).
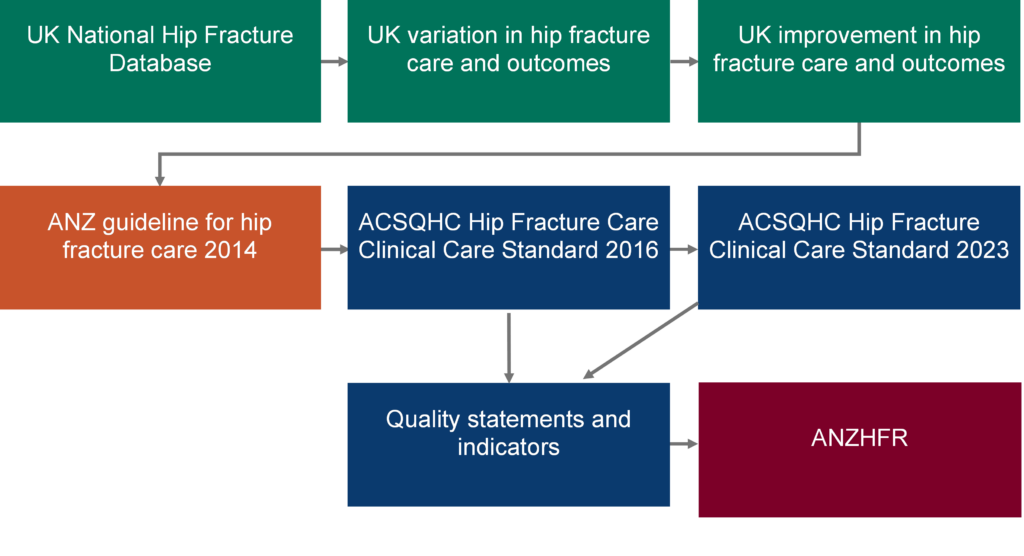
The ANZHFR is a clinical quality registry whose primary objective is to use data to drive change and improve outcomes for older people with a hip fracture (Box 1). The ANZHFR started collecting facility-level data in 2013 and patient-level data in 2015. Facility- and patient-level data have been designed to align with the quality indicators, facilitating annual reporting (Figure 1; Box 1).
| ANZHFR – Improving Outcomes for Older People after Hip Fracture |
| 1. Provide clinicians with timely and relevant data to drive quality improvement. |
| 2. Identify variation in processes and outcomes between hospitals and across health care systems. |
| 3. Evaluate hospital performance against the Australian and New Zealand guideline for hip fracture care and the ACSQHC Hip Fracture Clinical Care Standard |
| 4. Support sites to identify areas for improvement and provide opportunities for ideas exchange and learnings between sites. |
| 5. Contribute to the knowledge base of high quality and safe care for people with a hip fracture by providing the opportunity to address research questions. |
How the ANZHFR works: inclusion criteria, data collection, data linkage, reporting and monitoring
The ANZHFR collects data for people aged 50 years or older presenting to a participating hospital with a low trauma hip fracture. A minimum common dataset is supported by a data dictionary and each participating site is responsible for their own data collection and entry. Mortality data are obtained through linkage with the National Death Index in Australia and the Ministry of Health in New Zealand. In 2015, 24 hospitals contributed patient-level data, this has increased to 97 hospitals in 2022 with patient-level data for 16 395 patients. Quality indicators are reported annually and hospitals have access to a real-time dashboard to monitor their performance.
Using the ANZHFR for research: identifying wins and opportunities for improvement
In our recent study, we examined progress of ANZHFR early contributor hospitals — those that provided patient-level data before 1 January 2016 — against 11 quality indicators for hip fracture care using ANZHFR data (2016–2020).
Year-on-year improvements were demonstrated for the proportion of patients having pre-operative cognitive assessments (from 40% in 2016 to 70% in 2020) and nerve blocks before theatre (from 60% in 2016 to 84% in 2020). Prescription of bone protection medication on discharge also improved over time (from 20% in 2016 to 35% in 2020).
Other quality indicators demonstrated less consistent improvement or fluctuated over time; for example, emergency department stay of less than four hours, pain assessment and management within 30 minutes of presentation, surgery within 48 hours, and being offered the opportunity to mobilise early (on the day of, or the day after surgery).
Orthogeriatric assessment and unrestricted weightbearing had high attainment regardless of year, with minimal fluctuation. Pressure injuries increased in 2019 and 2020 (3.9% and 3.5% respectively) compared with 2016 (2.5%), but we are unable to determine if this is real or related to improved reporting.
Thirty-day mortality did not significantly change over time. The lack of meaningful improvement in key quality indicators that have been associated with reduced mortality may explain this finding; for example, surgery within 48 hours. In 2020, 365-day mortality was reduced when compared with 2016. However, this was based on a partial year of data and was at the beginning of the coronavirus disease 2019 (COVID-19) pandemic. Therefore, caution is needed interpreting this finding.
When we compared early contributor hospitals to all sites using ANZHFR Annual Reports, the early contributor hospitals had a higher level of quality indicator attainment for nerve blocks before theatre, orthogeriatric model of care, time to surgery, early mobilisation, unrestricted weightbearing and bone protection medication on discharge.
The study has some limitations that should be considered. The study is retrospective and the changes identified may be due to factors other than the ANZHFR. COVID-19 may have affected 2020 data. As data are entered by hospital staff and the validation rules have evolved over time, data entry errors may have occurred. Staffing changes can affect patient-level data entry, as was the case for one hospital in 2017. Finally, the ANZHFR offers educational/learning opportunities, such as HipFest (annual conference), HipCast (podcast) and newsletters which may influence hospital performance in an immeasurable way.
Implications and future directions
The ANZHFR and participating hospitals, including the early contributor hospitals, will continue to use data to monitor progress and implement improvement strategies to improve care for people who fracture their hip.
The improvements in quality indicators are encouraging, but also highlight opportunities for continued improvement. For example:
- Although the proportion of patients prescribed bone protection medication on discharge improved over time, only 35% of patients in the early contributor hospitals met this quality indicator in 2020.
- While the proportion of patients who are given the opportunity to mobilise was more than 90% in the early contributor hospitals in 2020, a new ACSQHC quality indicator introduced in 2023 shows that less than half of patients actually take steps (here). Recent research we’ve undertaken indicates that this is much lower for patients with cognitive impairment, with only 34% achieving early walking/stepping (here).
- Eighty-one per cent of patients had surgery within 48 hours in 2020 in the early contributor hospitals. However, the target introduced in 2023 is surgery within 36 hours.
In the United Kingdom and in a pilot trial in Australia, incentivised care improved outcomes (eg, time to surgery, length of stay, mortality) over and above the guideline, clinical care standard and audit model currently in place in Australia. Perhaps this is an opportunity to further improve care and outcomes, but health department and government support is needed.
In 2022, My Hip My Voice involved two pilot projects aimed at improving consumer engagement and represents the beginning of the ANZHFR’s aim to better understand, collect and improve outcomes that are valued by older people. This will be a continued focus for the ANZHFR.
Using the registry as a platform for research is a cost-efficient way of delivering new knowledge. The ANZHFR will continue to prioritise, support and seek research opportunities to better understand and improve hip fracture care and outcomes.
If your hospital operates on people with a hip fracture and is not yet participating in the ANZHFR, please contact the Registry manager Jamie Hallen at j.hallen@neura.edu.au or (02) 9399 1132 for information on how to get involved.
Dr Morag Taylor is a physiotherapist, Senior Research Fellow at Neuroscience Research Australia, a Conjoint Senior Lecturer, School of Population Health, Faculty of Medicine and Health, UNSW Sydney, and a part-time data analyst/research fellow with the ANZHFR.
Dr Lara Harvey is an injury epidemiologist, Senior Research Fellow and Team Lead for Data Linkage Studies at Neuroscience Research Australia and a Conjoint Senior Lecturer, School of Population Health, Faculty of Medicine and Health, UNSW Sydney.
Professor Jacqueline Close AM is a Geriatrician at the Prince of Wales Hospital, a Conjoint Professor with the School of Clinical Medicine, Faculty of Medicine and Health, UNSW Sydney and Co-Chair of the ANZHFR.
The authors would like to acknowledge the Australian and New Zealand Hip Fracture Registry and each participating site.
The statements or opinions expressed in this article reflect the views of the authors and do not necessarily represent the official policy of the AMA, the MJA or InSight+ unless so stated.
Subscribe to the free InSight+ weekly newsletter here. It is available to all readers, not just registered medical practitioners.
If you would like to submit an article for consideration, send a Word version to mjainsight-editor@ampco.com.au.

 more_vert
more_vert