Brain injury advocate Dr Bruce Powell is calling on all Australian governments to act on the recommendations of the recent Royal Commission into Violence, Abuse, Neglect and Exploitation of People with Disability.
In 2018, Dr Bruce Powell’s life changed in an instant. He was a highly experienced anaesthetist and Head of Department of the Intensive Care Unit at Rockingham Hospital in Western Australia when he became an intensive care patient himself.
Dr Powell was taking part in a charity cycling race on the Great Ocean Road in Victoria when he had a devastating accident. He broke his neck, lumbar spine, jaw, multiple ribs and both hands and woke up in hospital six days later.
However, it was the brain injury he acquired that ended his medical career and paved the way for him to become a researcher and advocate for the brain injury community.

In a Reflection article in today’s Medical Journal of Australia, he wrote about his experiences.
“We are forever grateful for the support provided by acute and rehabilitation teams of doctors, nurses, physiotherapists, occupational therapists, and neuropsychologists that have helped me to this point.
“My wife and I have had the pleasure of meeting other members of the acquired brain injury community across Australia, and those occasions are always emotional and poignant, reminding us of how lucky I am to survive and advocate for the brain injury community and other vulnerable groups,” Dr Powell said. said.
As Dr Powell’s rehabilitation continues, he is hopeful of making the best use of his skills, even if he can’t be in the career he loves.
However, following the publication of the final report into the Royal Commission into Violence, Abuse, Neglect and Exploitation of People with Disability in September this year, Dr Powell does not feel optimistic about meaningful systemic change.
The report outlined 222 recommendations, with topics including inclusive education, employment, housing and fair treatment in the criminal justice system. There was also a focus on improving services for First Nations people with disability and enhancing disability services through the National Disability Insurance Scheme.
Traumatic brain injury in Australia
Traumatic brain injury is a complex problem to address. It’s characterised by an injury to the brain caused by external force that varies in severity from mild to severe. New Zealand research estimates there are 790 cases per 100 000 person-years. Extrapolated, that means there are 190 000–200 000 cases per year in Australia, about 20 000 of those are moderate to severe. They found most traumatic brain injury is due to falls (38%), mechanical forces (21%), transport accidents (20%), and assaults (17%).
In Australia, MJA research found there were 16 350 people hospitalised in 2015–2020 with moderate to severe traumatic brain injuries. The mean age at admission was 50.5 years and 71.2% of patients were male.
The Royal Commission’s findings on brain injury
The Royal Commission report flagged that people with brain injuries experience barriers to accessing health care.
“From 2006 to 2015, there was no improvement in either survival rates or functional recovery for people with traumatic brain injury. This rehabilitation failure indicates a significant need for the development of more effective treatments that can decrease death rates and enhance the quality of life for brain injury patients, as well as alleviate the broader, adverse effects on families and society,” Dr Powell wrote in his Reflection.
People with brain injuries also experience higher rates of violence: “people with head injury, stroke and brain damage [73%] … [have experienced] violence since age 15,” the Royal Commission report noted.
First Nations people with a disability, particularly women, are even more at risk.
“Over one-third of First Nations women with head injury, stroke or brain damage, 27 per cent with intellectual disability and 26 per cent with psychological disability experienced physical harm or threat in the previous 12 months,” the report stated.
The federal, state and territory governments have until 31 March 2024 to publish their written responses to the Commission’s recommendations. Dr Powell hopes that the Australian jurisdictions care enough about the disabled community to act quickly.
“Will the governments tell our communities which recommendations they plan to act on, which they do not, and why? Will the needs of the brain injured, and other vulnerable communities trigger bipartisan collaboration and cooperation?” he asked.
In the meantime, he thanks those working in the sector.
“We will keep faith in the commitment and skills of our health care professionals and their remarkable work for the vulnerable such as those with brain injuries,” he said.
Subscribe to the free InSight+ weekly newsletter here. It is available to all readers, not just registered medical practitioners.

 more_vert
more_vert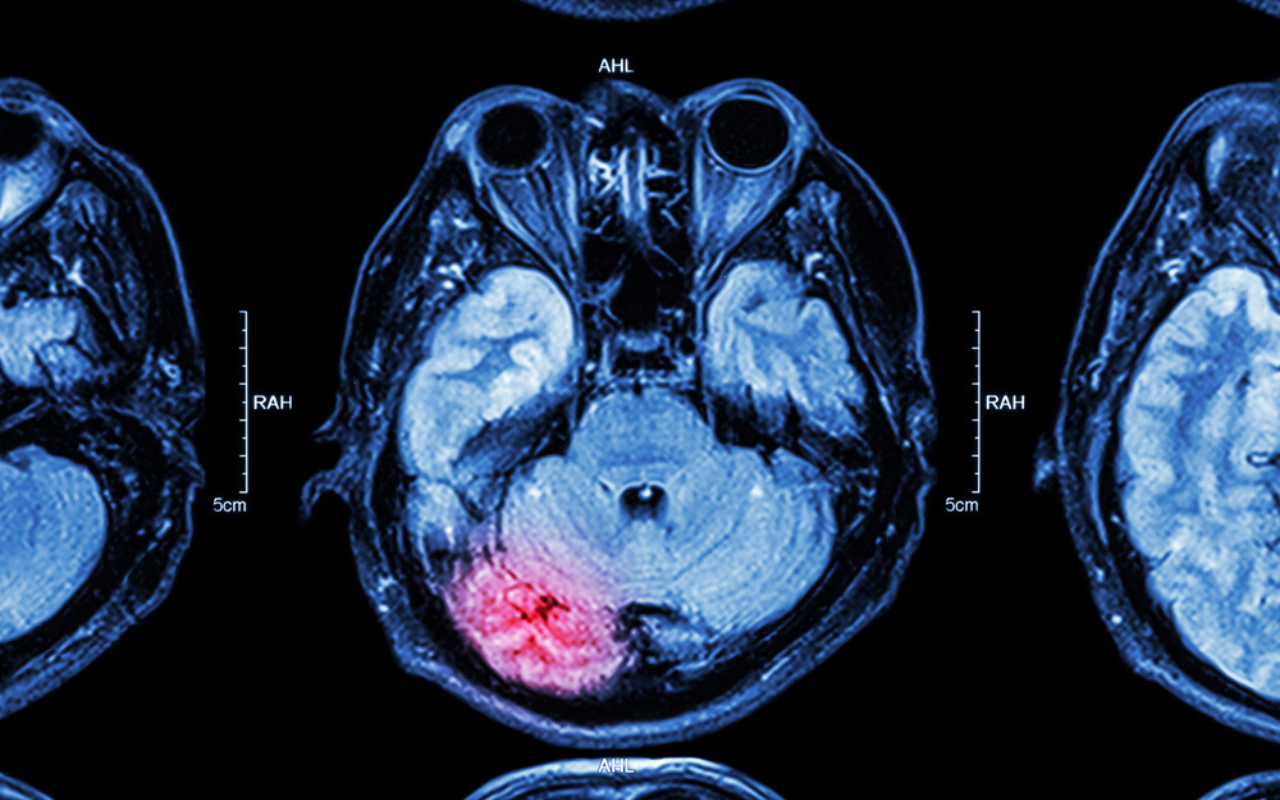
Dr Powell has written a useful and provoking article, but if hoping for a productive political response, I think self help will be better than waiting.
Rehab often involves restoring lost function, retraining alternate function, strengthening weakened parts etc and most of this will be repetitive stuff that is hard to stay with.
Professional help to point the direction and a measuring system to accurately assess progress are both important.
For moral support look to family, friends, fellow disabled, disabled groups.
Don’t forget laughter. It really is good medicine.
Don’t forget laughter. It really is good medicine. (Worth repeating)