Time is running out for Australia to establish a coordinated national response to the rise of antibiotic-resistant bacteria infections.
A national response is required to minimise the growing risk of carbapenemase-producing Enterobacterales (CPE) to Australia’s health care system, according to a Perspective published in the Medical Journal of Australia today.
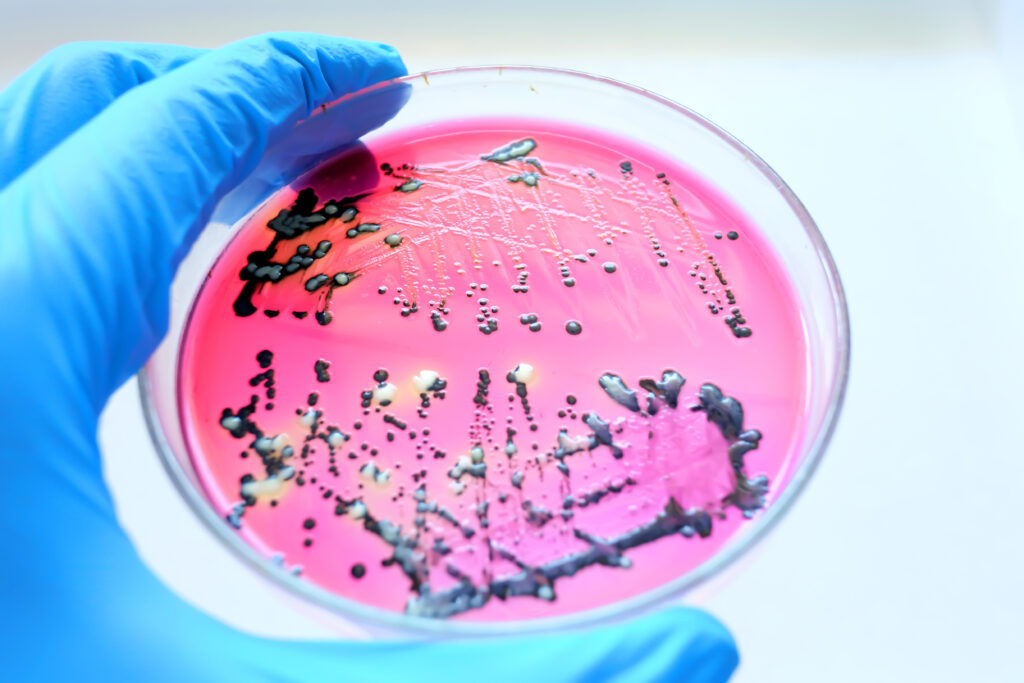
Enterobacterales is a group of bacteria that normally live in the human gut and include Escherichia, Klebsiella and Salmonella.
Authored by SA Pathology’s Dr Lito Papanicolas and colleagues, the Perspective states that when these bacteria produce enzymes, called carbapenemase, they become resistant to most types of antibiotics.
“Worryingly, the number of bacterial pathogens that are associated with antibiotic treatment failure due to acquired resistance is growing rapidly,” Dr Papanicolas and her colleagues wrote.
“Among these, CPE is arguably the most concerning.”
The clinical and economic impact
The article authors highlight the impact that CPE is having around the world, especially in antibiotic treatment outcomes for sepsis.
“For a bacterial infection resulting in septic shock, every hour of ineffective antibiotic therapy results in a 7.6% relative reduction in survival,” they wrote.
In practice, current empirical antibiotic regimens are not tailored to cover CPE, a factor contributing to high mortality rates for CPE infections.”
The economic impact is also significant, with recent outbreaks in the United Kingdom and France costing their respective health systems up to AU$2 million.
Economic estimates in Australia are limited but have suggested that individuals affected by CPE have six times higher health care costs that those not affected.
“A recent [World Health Organization] report projected a cumulative total of 5.2 million antimicrobial resistance-related deaths in the Western Pacific region from 2020 to 2030, with economic costs forecast to reach US$148 billion, indicating the enormity of the problem in our region,” the authors wrote.
Better surveillance needed
Although current estimates suggest that Australia’s CPE burden is low, Dr Papanicolas and colleagues argue that time is running out for a coordinated national response to this growing threat.
They have called for nationally consistent surveillance of CPE infections in Australia to combat the risk they pose to our health care system.
“Currently, CPE infection is only notifiable in five of the eight states and territories, and consequently, CPE burden is likely underestimated,” they wrote.
The authors also note the need for greater funding to support laboratory detection of CPE and pathogen genomics.
“There is also no coordinated approach to comparative genomic analysis fundamental to detecting hypervirulent strains, and clonal and plasmid-borne outbreaks,” they wrote.
“For these reasons, our understanding of CPE epidemiology, the risks posed, and the effectiveness of prevention and control measures are limited.”
The authors are hopeful that the recently established Australian Centre for Disease Control is well placed to be a national coordinating body in the fight against CPE.
“Australia now has a unique opportunity to take coordinated national action to prevent the spread of CPE,” the authors conclude.
Read the Perspective in the Medical Journal of Australia.
Subscribe to the free InSight+ weekly newsletter here. It is available to all readers, not just registered medical practitioners.

 more_vert
more_vert
Is there any person who is looking at this work on antimicrobial resistance and the pharmacy antibiotic prescribing programs together?
The Australian CDC is only currently being stood up. It is not yet established, however attention to antimicrobial resistance will be one of its key foci.