By bridging the gap between urban and rural health care, telestroke helps give every patient with stroke the best chance of a full recovery.
Stroke is common and frequently devastating, affecting thousands of Australians each year (here).
Telehealth services are revolutionising access to stroke diagnosis and treatment in rural communities, leveling the playing field for patients who may not have previously had access to expert care (here).
In this article, we explore the ability of telestroke services to improve stroke diagnosis and outcome.
Setting the stage: the reality of stroke in Australia
In 2020 there were over 445 000 stroke survivors in Australia, with approximately 27 000 new stroke diagnoses reported that year (here).
Without significant advances in stroke prevention, these numbers are projected to rise even further by 2050, with an estimated 50 600 annual strokes and over 819 000 Australian stroke survivors (here).
Rural and regional communities bear a disproportionate burden of stroke, with a risk of stroke 17% higher than their metropolitan counterparts (here). Additionally, stroke-related in-hospital mortality rates are alarmingly higher in these areas (here).

The struggle to bring specialist stroke care in rural hospitals
Before the advent of telestroke, regional hospitals often faced challenges in accessing specialised care for hyperacute stroke therapy.
With workforce shortages and limited resources, many rural medical facilities were unable to provide the level of expertise required for safe and timely stroke treatment (here).
As a result, hyperacute stroke care, if available at all, was primarily provided by general physicians, emergency physicians, and general practitioners.
Enter telestroke: bridging the gap
Fortunately, telehealth-based stroke neurologist support, also known as “telestroke”, has emerged as a game-changer in the fight against rural stroke treatment inequities.
Telestroke services have been implemented worldwide (here), and they have proven to be a powerful tool in providing expert advice to regional hospitals.
One noteworthy example is the Victorian Stroke Telemedicine (VST) program, which considerably improved treatment metrics and patient outcomes through telehealth support.
The birth of the South Australian Regional Telestroke Service
In South Australia, the need for specialised care in regional hospitals led to the creation of the South Australian Regional Telestroke (SAT) Service, Australia’s second 24/7 statewide service. Launched on 4 June 2018, this innovative program aimed to provide 24-hour telehealth support to patients with hyperacute stroke presenting within 24 hours of onset at three major regional stroke hospitals (here).
How telestroke works
The SAT Service operates through a secure videoconferencing system, allowing rural medical practitioners to connect with an on-call stroke neurologist at any time of day.
When a patient meets the code stroke criteria (as per ROSIER criteria), they become a priority for ambulance transfer to their local regional stroke hospital.
Hyperacute multimodal computed tomography (CT) imaging, such as non-contrast brain CT scan, CT angiography, and CT perfusion imaging, is performed and the telestroke neurologist is contacted for a videoconference call.
During the videoconference, the stroke neurologist can assess the patient, review the neuroimaging, and provide an accurate diagnosis.
This real-time communication enables the initiation of hyperacute stroke management, including thrombolysis (clot-dissolving treatment) and, if indicated, transfer to a metropolitan hospital for endovascular clot retrieval.
Even for patients who do not meet the code stroke criteria but still present acutely (within 24 hours), acute stroke management advice and telestroke consultation are provided.
Measuring the impact: assessing quality of care and stroke outcomes
To evaluate the SAT project’s impact, we conducted a mixed-methods historically controlled cohort study.
Data were collected for six months before implementation and 18 months after implementation.
The study focused on several key aspects, including quality of care indicators (eg, door-to-needle time, telesupport availability, allied health professional input, and adherence to best practice guidelines for secondary prevention) and patient mortality up to a year after stroke.
The positive effect of telestroke: improving stroke care metrics
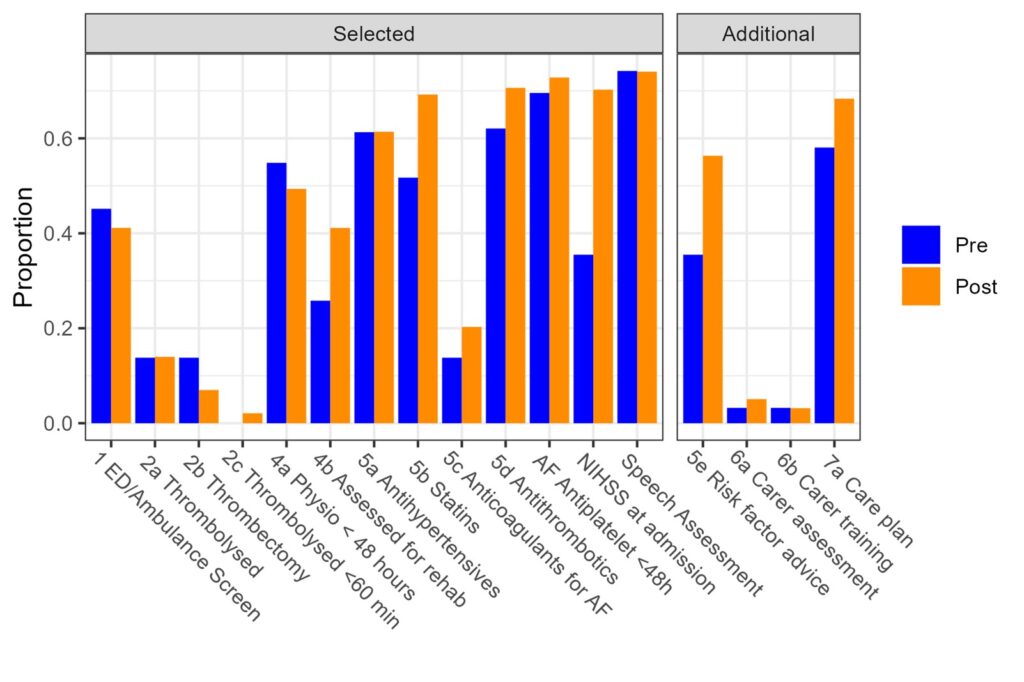
The introduction of the SAT Service led to improvements in stroke care metrics, with most quality indicators showing improvement (Figure 1).
The composite quality indicator score, which takes into account multiple care aspects (Figure 1), was significantly higher during the intervention period than the control period (selected indicators: adjusted change, 0.069; 95% confidence interval [CI], 0.004–0.134; P = 0.04; all indicators: adjusted change, 0.073; 95% CI, 0.005–0.140; P = 0.03). This includes faster onset-to-presentation times and improved ambulance response facilitated by expert telestroke consultation.
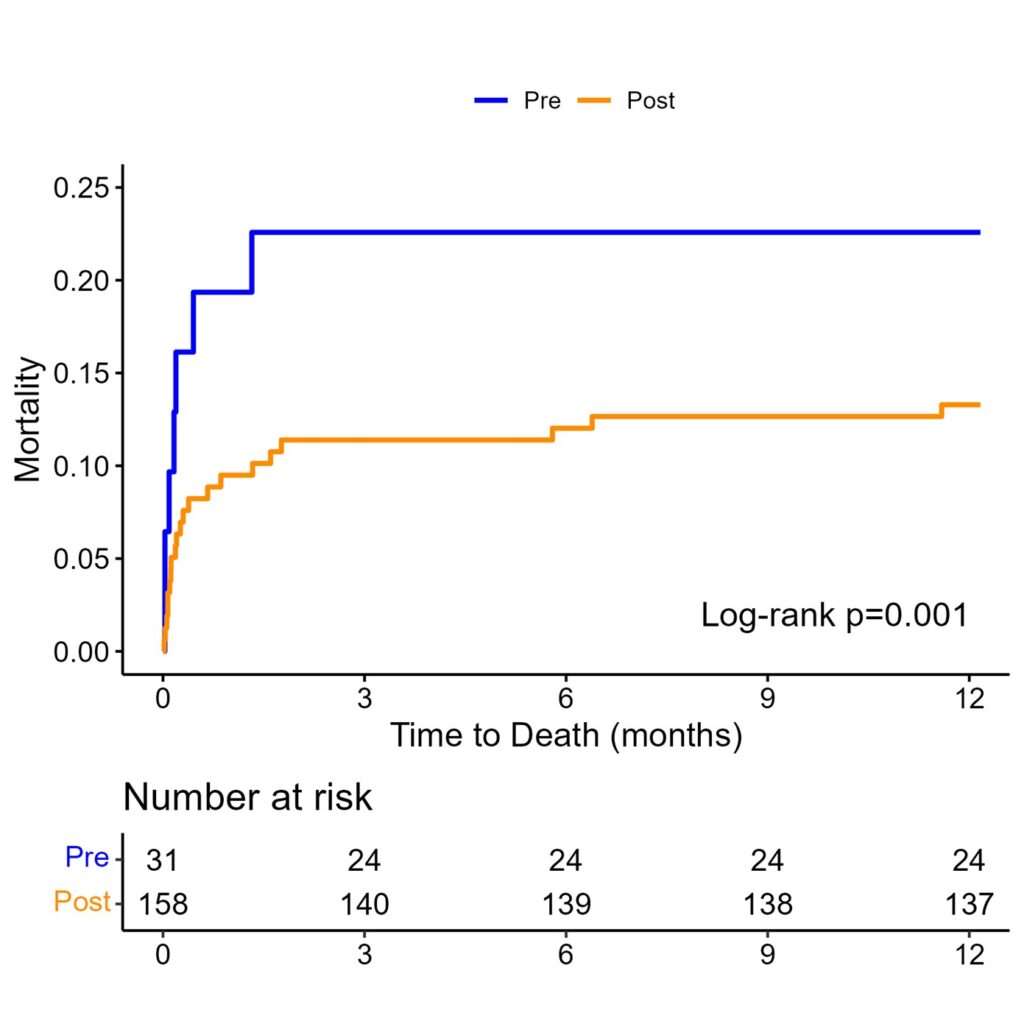
In association and possibly as a result, stroke survival rates showed a positive trend, with mortality rates decreasing significantly in the short and medium term after the introduction of telestroke (23% pre-implementation v 13% post-implementation; adjusted hazard ratio, 0.58; 95% CI, 0.44–0.76; P < 0.001) (Figure 2).
Beyond the acute intervention: the broader impact of telestroke
The SAT Service facilitated accurate stroke subtyping and secondary prevention, providing comprehensive treatment plans and better rehabilitation access for patients.
Correct diagnosis of stroke mimics, stroke, and stroke subtype facilitates optimised secondary prevention, minimises unnecessary treatment and investigation, and prevents the adverse psychological financial and insurance impacts should stroke be otherwise erroneously diagnosed.
Additionally, improved guideline adherence and carer education contributed to enhanced stroke care outcomes.
The future of telestroke in regional Australia
Our findings strongly support the long term implementation and expansion of telestroke services in regional Australia.
Recent media announcements from Western Australia and Queensland now foreshadow complete national coverage (here and here).
I argue that every CT-capable hospital in regional Australia should be considered as a telestroke-capable stroke hospital.
Current pilot projects in Victoria (here) and New South Wales (here) are examining bringing creating “virtual stroke units” in regional centres, to further reduce stroke-related death and disability beyond the hyperacute phase.
The success of the SAT Service paves the way for similar initiatives in other conditions. Although on-site specialist care may be impossible to provide in many regional centres, analogous specialist-led telemedicine regional services can reduce the “postcode lottery” inequities in service delivery.
Conclusion
Telestroke has emerged as a powerful tool in transforming stroke care for rural and regional Australians. With improved care metrics and reduced mortality rates, this telehealth-based service is proving to be a game-changer in the fight against stroke.
By bridging the gap between urban and rural health care, telestroke helps give every patient with stroke the best chance of a full recovery.
State and federal government support is welcomed in ensuring that there is equity of telestroke access nationwide.
Dr Rudy Goh is a Neurology Advanced Trainee at the Central Adelaide Local Health Network.
The statements or opinions expressed in this article reflect the views of the authors and do not necessarily represent the official policy of the AMA, the MJA or InSight+ unless so stated.
Subscribe to the free InSight+ weekly newsletter here. It is available to all readers, not just registered medical practitioners.
If you would like to submit an article for consideration, send a Word version to mjainsight-editor@ampco.com.au.

 more_vert
more_vert