The first national study to examine the impact of COVID-19 on patients with cancer shows the importance of Australian research in examining the impacts of this disease on specific populations.
To date, the impact of coronavirus disease 2019 (COVID-19) on patients with cancer in Australia, some of the nation’s most vulnerable, has been unknown.
International reports in the early stages of the COVID-19 pandemic in 2020 were cause for concern for patients with cancer – in one large study of patients with blood cancer, the mortality rate from COVID-19 was found to be 38%.
However, these studies had short follow-up periods and occurred in different public health contexts (the United States, Europe, the United Kingdom) where community COVID-19 case numbers were substantially higher.
Our unique response
In many ways, Australia is unique from the rest of the world and so was its response to the COVID-19 pandemic.
Wearing of face masks, intensive testing, mandatory quarantine, physical distancing, and closure of international borders meant that COVID-19 cases were relatively infrequent until late 2021.
From December 2021 onwards, these restrictions were lifted and the highly transmissible Omicron variant of the causative virus, the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), dominated cases in the community.
At the same time, more than 90% of the Australian population were considered fully vaccinated, and there was accessible, rapid COVID-19 testing and early outpatient therapies for people at risk of severe COVID-19, including patients with cancer.
The effectiveness of antiviral therapies and vaccination has been demonstrated in the general population.
Recommendations for immunosuppressed patients, however, have been extrapolated and largely based on these data.
What we studied
To our knowledge, our study is the first multicentre, national study to examine the impact of COVID-19 on patients with cancer in Australia, spanning from March 2020 to April 2022.
Fifteen cancer health care services across five capital cities and three major regional centres participated, with 620 patients with cancer and COVID-19 included.
The median age was 64 years; there were similar numbers of males and females and representation of patients with solid organ tumours (392/620, 63.2%) and blood cancers (228/620, 36.8%).
Many of these patients had already received COVID-19 vaccination (75% with one dose or more) and more than half were receiving anticancer therapy at the time of COVID-19 diagnosis.
Short time to COVID-19 diagnosis
The most common symptoms included cough, fever and coryza.
Most patients were diagnosed by nasopharyngeal swab polymerase chain reaction (PCR) test, and there was a median time from symptoms to diagnosis of one day.
This likely had a positive follow-on effect to alerting their health care team or family doctor of the diagnosis and to enable at-home monitoring as well as accessing early antiviral therapy.
Patients with blood cancer who test positive
Consistent with clinical experience, we found that patients with blood cancers tested positive for COVID-19 on PCR test for a considerably longer time than those with solid organ tumour (median, 21 v 7 days) even as symptoms resolved.
This prolonged shedding of virus, usually related to deficiencies in antibody production, continues to remain a clinical and infection control challenge for clinicians. The optimal management of these patients, often receiving B cell-depleting treatments, requires further study.
Risk factors for oxygen therapy have been identified
One-third of patients required hospital care (210/620, 33.9%), and some of these patients (85/210, 40.5%) needed oxygen therapy.
We assessed for risk factors that might lead to requiring oxygen support, as this is a marker of more severe COVID-19. Increasing age, male sex, and not receiving any outpatient antiviral therapy was shown to lead to an increased risk of requiring oxygen.
Patients with metastatic cancers were also more likely to need oxygen if they contracted COVID-19. We did not find any specific chemotherapy or immune suppression to predict needing oxygen.
Diagnosis during the Omicron wave was also protective and associated with a lower risk of needing oxygen.
This has been found in the general population, whereby the Omicron variant has been found to be less severe – probably related to it replicating in the upper airways more than the lower airways.
Patients with blood cancers did require higher levels of support (ventilation, intensive care unit) compared with patients with solid organ tumours.
This is expected given that they receive more aggressive therapies, leading to more immunosuppression.
However, the rates of death related to COVID-19 at 100 days after diagnosis were relatively low for both groups (7.3% for blood cancers and 3.8% for solid organ tumours), in particular in comparison to the early reports during 2020.
COVID-19 severity decreased over time
One of the most encouraging findings of our study is that the severity of COVID-19 in patients with cancer decreased over time.
Hospitalisation, oxygen therapy, ventilation and intensive care unit requirements all decreased, along with a decrease in all-cause mortality at 100 days after diagnosis (from 26% in 2020 to 8% in 2022).
Most patients in our cohort were diagnosed during the Omicron wave in early 2022, mirroring the general population in Australia.
This coincided with increased awareness among clinicians, availability of early antivirals and high vaccination rates.
We found that nirmatrelvir/ritonavir reduced the need for oxygen therapy, supporting previous findings of its benefit in higher risk and older patients.
COVID-19 recommendations in 2023 for patients with cancer
Our study provides hope for patients with cancer as the COVID-19 pandemic continues in a world where public health measures have largely been wound back.
Although COVID-19 should still be respected, it does not necessarily need to be feared.
In 2023, most patients will now have been exposed to and/or infected with SARS-CoV-2.
There is clear evidence from our results and other studies that the Omicron variant, including the most recent subvariants, is less severe.
This is likely related to the virus itself and a concept known as “hybrid immunity”, whereby vaccination and infection enhances protection against further infection and severe COVID-19.
Improved immunity
Although there appears to be increasing evasion of Omicron subvariants to vaccination and monoclonal antibodies, meaning increased chance of infection, there is still good cross-protection from T cell immunity, which is known to decrease the severity of illness.
In addition, even in patients who are heavily immunosuppressed with blood cancers, and may not make antibody responses to vaccination, T cell immunity from infection and/or vaccination appears to be preserved.
Therefore, severely immunosuppressed adult patients (aged 18 years or older) are still highly recommended to receive three doses of COVID-19 vaccine as the primary course, with the third dose two months after the second vaccine. From February 2023, booster doses for severely immunocompromised patients are now recommended every six months since the last vaccination or COVID-19 infection. There is no requirement for a specific number of booster doses.
Robust antivirals
We have robust antiviral therapies that have remained effective despite the evolution of SARS-CoV-2, are readily available, and are listed in the Pharmaceutical Benefits Scheme for eligible people.
Potential medication interactions should be checked before prescription of nirmatrelvir/ritonavir and may require specialist pharmacy and care provider input.
The earlier the better for these antivirals, but within five days of symptom onset is the current criterion for starting nirmatrelvir/ritonavir.
Remdesivir is another option if outside of this window (within seven days of symptoms) or there are prohibitive drug–drug interactions, but it requires intravenous administration for now – an oral formulation is in process.
Therefore, rapid diagnosis of COVID-19 whether by PCR test or rapid antigen testing (RAT) and medical follow-up remains important for people with cancer.
Importance of this research
In summary, our study has provided a comprehensive description of COVID-19 in patients with cancer in Australia and underpins the importance of performing local research.
We advocate for ongoing vigilance for people with cancer, including optimising vaccination status, and prioritising them for testing to seek a timely diagnosis with the development of symptoms and, if eligible, early antiviral therapy.
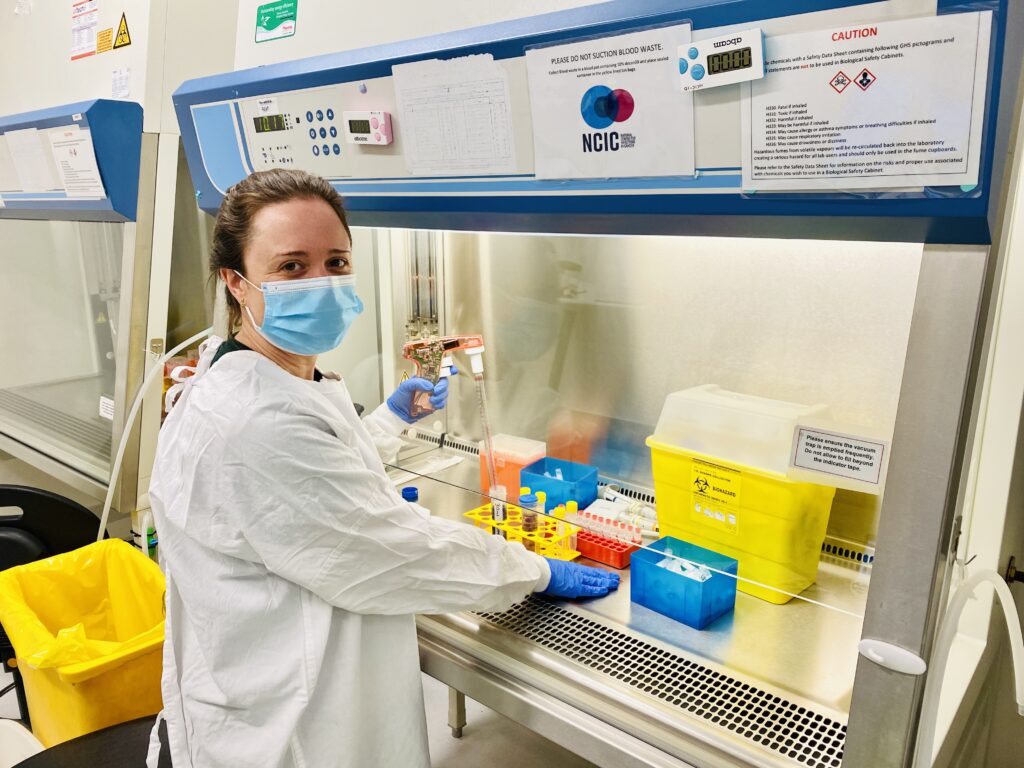
Dr Victoria G Hall is an Infectious Diseases Physician and PhD candidate at the Sir Peter MacCallum Department of Oncology, University of Melbourne and National Centre for Infections in Cancer, Peter MacCallum Centre.
Dr Michelle K Yong is an Infectious Diseases Clinician-Researcher at the Department of Infectious Diseases, Royal Melbourne Hospital and National Centre for Infections in Cancer, Peter MacCallum Centre.
Professor Monica A Slavin is an Infectious Diseases Clinician-Researcher, the Director of the National Centre for Infections in Cancer, Peter MacCallum Centre and Immunocompromised Host Service at Royal Melbourne Hospital.
Associate Professor Benjamin W Teh is an Infectious Diseases Clinician-Researcher at the Sir Peter MacCallum Departments of Oncology, University of Melbourne and National Centre for Infections in Cancer, Peter MacCallum Centre.
The authors would like to acknowledge Beatrice Z Sim, Chhay Lim, Christopher Hocking, Teddy Teo, Naomi Runnegar, Peter Boan, Christopher H Heath, Natalie Rainey, Megan Lyle, Christopher Steer, Eunice Liu, Cassandra Doig, Kate Drummond, Patrick GP Charles, Katharine See, Lyn-Li Lim, Omar Shum, Narin Bak, Sue-Anne Mclachlan, Kasha P Singh, Nicholas Laundy, Jenny Gallagher, Marcelle Stewart, Natalie R Saunders, Emily Klimevski, Jessica Demajo, Gemma Reynolds, Karin A Thursky, Leon J Worth, Timothy Spelman for their valuable contributions to this multicentre, national study.
The statements or opinions expressed in this article reflect the views of the authors and do not necessarily represent the official policy of the AMA, the MJA or InSight+ unless so stated.
Subscribe to the free InSight+ weekly newsletter here. It is available to all readers, not just registered medical practitioners.
If you would like to submit an article for consideration, send a Word version to mjainsight-editor@ampco.com.au.

 more_vert
more_vert