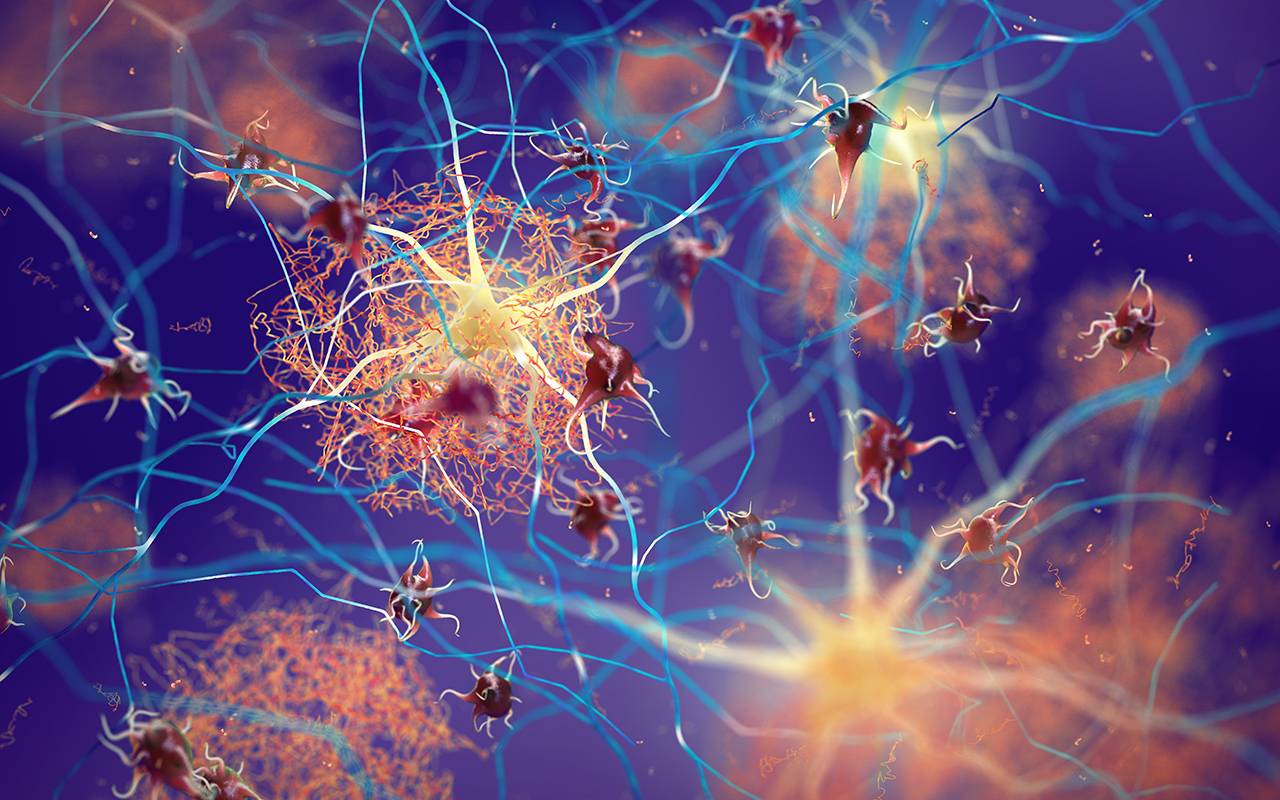
A HIGH-cost Alzheimer drug that virtually eliminates amyloid plaques but without convincing evidence of clinical benefits has divided Australian experts, as the Therapeutic Goods Administration (TGA) considers an application for its registration.
Aducanumab, a monoclonal antibody, is considered the first disease-modifying Alzheimer therapy because it reverses ß-amyloid deposition – widely regarded as the most likely cause of the disease.
The drug was approved by the US Food and Drug Administration (FDA) in June 2021 – the first new treatment for Alzheimer disease (AD) in almost two decades. It is indicated for patients with mild cognitive impairment or dementia stage of disease.
However, the approval defied the advice of the FDA’s own expert panel, which found there was insufficient evidence that it slowed cognitive decline. Three committee members resigned in protest and the FDA commissioner was compelled to request an independent inquiry to determine whether manufacturer Biogen had undue influence over the drug’s approval process.
The pathway to aducanumab’s approval has been unconventional, to say the least.
Two global phase 3 trials of the drug, ENGAGE and EMERGE, were discontinued in March 2019, when an independent data monitoring committee found they were unlikely to meet primary endpoints.
Six months later, the company that produces aducanumab announced that new analysis of a larger dataset, which became available after the pre-specified futility analysis, showed that the drug reduced clinical decline in patients with early AD and that, on this basis, it would apply for FDA approval. The new positive results, the company said, were driven primarily by greater exposure to high dose aducanumab in the larger dataset, as compared with data available when the trials were halted.
The FDA noted that while evidence from the updated EMERGE and ENGAGE studies were mixed, both “consistently and very convincingly reduced the level of amyloid plaques in the brain in a dose- and time-dependent fashion”.
“It is expected that the reduction in amyloid plaque will result in a reduction in clinical decline,” the FDA said.
On this basis, the FDA approved aducanumab through an “accelerated pathway”, which enables medications for serious or life-threatening illnesses to be approved based on a surrogate, rather than a primary clinical endpoint.
The FDA has given Biogen 9 years to conduct a post-approval clinical trial to verify the drug’s clinical benefit.
In the meantime, aducanumab is costing Americans US$28 200 per patient per year (AUD$40 000).
In a critical Perspective published in the MJA, Australian experts, led by Professor Ashley Bush, Director of the Melbourne Dementia Research Centre at the Florey institute of Neuroscience and Mental Health, likened the evidence underpinning the FDA’s decision to “winning a Texas sharpshooter contest by drawing a bull’s-eye around a bullet hole”.
“Premature approval without evidence of clinically meaningful benefit from controlled clinical trials is costly to government as well as patients (who are exposed to side effects), may make it harder to recruit to experimental placebo-controlled clinical trials, and could divert research funding away from the development of more effective treatments,” they wrote.
“Disease-modifying therapies for AD are urgently needed, but science, not desperation, should guide the approval process,” they added.
Speaking with InSight+, Professor Bush said he no longer believed anti-amyloid therapies held much promise.
“There have been over 30 phase 3 clinical trials targeting amyloid, and many have removed amyloid, but even with aducanumab, which very effectively removes amyloid, the clinical benefits are even more subtle than with the available drugs – acetylcholinesterase inhibitors and the [N-methyl D-aspartate (NMDA)] antagonist memantine,” he said.
“Aducanumab also takes much longer to work than the medicines already available, with a slight slowing of deterioration after 18 months treatment, if the data can be believed.”
Professor Bush noted aducanumab was strongly associated with a poorly understood but potentially serious adverse event known as amyloid-related imaging abnormality (ARIA), which can cause brain bleeds.
The most common, oedematous form of the condition, ARIA-E, occurred in 35% of the treatment cohort, compared to 3% on placebo. Professor Bush said this had the effect on “unblinding” 35% of the cohort, potentially influencing the results of the two trials.
Professor Bush commented:
“There are concerns about the tendency of anti-amyloid drug candidates to accelerate brain volume loss, but this data has not been reported by either Biogen or the FDA, despite it being a pre-specified endpoint.”
Aducanumab is just one of a number of anti-amyloid drugs for AD, with ongoing trials of lecanemab and donanemab.
“We have to be open minded about the possibility that removing amyloid could be beneficial, but it also might not be, and there may still be better therapeutic targets, such as tau or iron deposition,” said Professor Bush.
In contrast, Professor Ralph Martins, Foundation Chair in Ageing and Alzheimer’s Disease at Edith Cowan University and Professor of Neurobiology at Macquarie University, said he and many colleagues remained strongly convinced of the amyloid hypothesis and hoped aducanumab would soon be approved in Australia and listed on the Pharmaceutical Benefits Scheme.
“There is a huge amount of evidence in the literature to support the amyloid hypothesis,” he said.
“For example, people with Down syndrome who commonly go on to get dementia have an extra copy of the amyloid gene, and there are also two major genes intimately linked to the amyloid pathway – APP and PS1 – and these occur in a vast majority of familial onset cases.”
Professor Martins said there was a convincing explanation for why aducanumab had not been linked with dramatic clinical improvements in trials, despite clearing amyloid.
“It is because of the cascade of events that contribute to AD,” he said. “The amyloid deposition comes first, which triggers a series of events, such as tau build-up, and once those events take place, the brain can be damaged irreparably.”
“The horse has already bolted for many patients in the clinical trials,” he said, “However, anti-amyloid therapies are likely to be most useful in early stage and particularly pre-clinical AD.”
Professor Martins said the FDA had rightly recognised the urgent burden of AD, and that aducanumab was effectively targeting the disease’s underlying biology.
“Maybe the approval was a bit too early, but when do we start?” he said. “If you ask families, everyone would say they want it now.”
Professor Martins said patients required a [positron emission tomography (PET)] amyloid scan to confirm the presence of amyloid before undergoing aducanumab therapy. They should also undergo [magnetic resonance imaging (MRI)] monitoring to look for ARIA, with closer monitoring of patients with the APOe4 gene because they were at increased risk of side effects.
If aducanumab becomes available in Australia for patients with mild AD, it is estimated that around 150 000 Australians would be eligible.
Professor Bush and colleagues estimated that if all of these patients were treated under the Pharmaceutical Benefits Scheme (PBS), PBS expenditure would increase by about 50%. Real costs would be much higher, they said, taking into account resources needed for infusions, MRI monitoring, and management of adverse events.
One thing the Australian experts do agree on is the cost of the drug.
Professor Martins said the drug’s price tag had been a sour point for many doctors who welcomed the FDA approval.
“It’s just crazy, unacceptable,” Professor Martins said. “Many medical centres in the US have been choosing not to use aducanumab in protest against its cost, and I’m hoping that will have a positive effect in bringing the cost down, together with the release of some even more powerful anti-amyloid drugs that are now in the pipeline,” he said.
A TGA spokesperson said the independent expert Advisory Committee on Medicines was scheduled to consider Biogen Australia’s application in April, with the TGA to make a regulatory decision later in 2022.
Also online at mja.com.au
Podcast: Dr Stephen Russell, University of Alabama, and Dr Maja Artandi, Stanford University, talk about how to optimise video telemedicine examinations by partnering with patients … FREE ACCESS permanently.
Perspective: GP supervisors in Australia: a cornerstone in need of repair
Ingham and Johnson; doi: 10.5694/mja2.51411 … FREE ACCESS for 1 week.

 more_vert
more_vert