The National Obesity Strategy is a welcome policy development in Australia. However, by its own admission, the targets are aspirational and require significant action across many aspects of society
AS the well known saying goes, prevention is better than cure. Preventive health care is defined by the Royal Australian College of General Practitioners (RACGP) as “the prevention of illness, the early detection of specific disease, and the promotion and maintenance of health”.
However, the provision of such care is dependent on much more than clinical knowledge and skills. Supportive health policy is needed to ensure that GPs can provide high quality preventive care and address barriers such as out-of-pocket costs, which are often not possible to overcome at an individual practitioner or practice level.
Overweight and obesity in Australia
Overweight and obesity are a major contributor to disease burden in Australia, second only to tobacco in 2018. Approximately one in four children (2–17 years old) and two in three adults were living with either overweight or obesity in 2017–2018. Overweight and obesity prevalence among children rises with increasing age, and by the time they reach adolescence, almost one in three are living with overweight or obesity. The development of obesity is multifactorial, influenced not only by biological but also environmental contributors.
As the most frequently consulted health care professionals in Australia, GPs can play an important role in preventing excess weight gain among children through the provision of preventive care.
Impact of health policy on clinical practice
Health policy – described as “courses of action (and inaction) that affect the set of institutions, organizations, services and funding arrangements of the health system (both public and private)” – can shape clinical practice. Although a clinician’s knowledge and skills are core, as demonstrated by the levels in an ecological model (Figure), multiple factors can influence a GP’s clinical consultation. Examples include colleagues, patients, infrastructure of the practice where it occurs and, importantly, the overarching public policy environment.
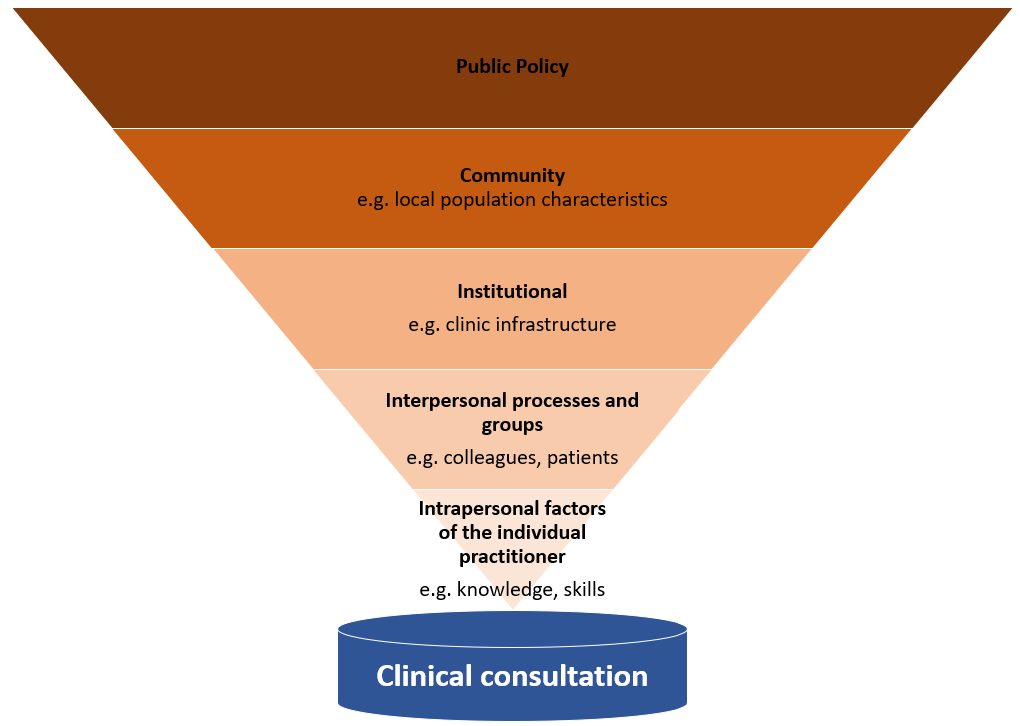
Figure: Examples of influences on a GP’s day-to-day clinical practice using an ecological model adapted from McLeroy et al
The now defunct Healthy Kids Check (HKC) was an example of a policy-enabled opportunity for GPs to offer a specific preventive health consultation to Australian preschoolers, funded through Medicare. Before discontinuation in 2015, the HKC was taken up by 50% of the eligible population and provided an opportunity to address excess weight gain among these young children. Although not a panacea, it demonstrated that health policy can nevertheless be a critical enabling factor for more reimbursed services, encourage professional development, and increase interest in the practice of preventive care.
Despite this importance of policy settings, as of late 2021, there were no publicly available documented policies to specifically support GPs to provide obesity prevention services for children and their families. We conducted a scoping review to identify Australian health policy documents which linked the prevention of childhood obesity through the promotion of healthy weight maintenance to the clinical practice of GPs. Secondarily, the review also sought documents supporting similar practice for paediatricians and maternal child health nurses in recognition of the broader group of commonly consulted child health professionals. However, a search incorporating both grey and peer reviewed literature, including websites of Australian federal and state and territory health departments and relevant professional representative organisations (eg, the RACGP), revealed a paucity of policy guidance supporting GPs to prevent childhood obesity. Of the 867 documents screened, only one document met the selection criteria and it had a particular focus on paediatricians.
An opportunity for change
In March 2022, the National Obesity Strategy was released under the auspices of the Health Ministers meeting, representing all Australian state and territory Health Ministers and the federal Minister for Health and Aged Care. The Strategy’s goal is for “more people to maintain a healthy weight”, including the reduction of overweight and obesity among children and adolescents by 5% or more by 2030. The Strategy is linked to the National Preventive Health Strategy 2021–2030, which was launched 4 months earlier, and includes the same target for reduction of overweight and obesity among children and adolescents.
The National Obesity Strategy is a welcome policy development in Australia. However, by its own admission, the targets are aspirational and require significant action across many aspects of society. Nevertheless, the National Obesity Strategy signals recognition of obesity as a policy priority and willingness at both state/territory and federal political levels to address this, presenting a rare opportunity to develop health policies that will support the prevention of childhood obesity in general practice.
Michelle Gooey, Health and Social Care Unit, School of Public Health and Preventive Medicine, Monash University, Melbourne.
Alexandra Chung, Health and Social Care Unit, School of Public Health and Preventive Medicine, Monash University, Melbourne.
Helen Skouteris, Health and Social Care Unit, School of Public Health and Preventive Medicine, Monash University, Melbourne, and Warwick Business School, University of Warwick, Coventry, UK.
Elizabeth Sturgiss, School of Primary and Allied Health Care, Monash University, Melbourne.
Funding and competing interests
This work was supported by a National Health and Medical Research Council (NHMRC) postgraduate scholarship for Michelle Gooey (2021–2023; GNT2005401), the Medical Research Future Fund (MRFF APP1199826) for Alexandra Chung, and an NHMRC Investigator Grant, 2020–2024 for Elizabeth Sturgiss. Outside of the submitted work, Michelle Gooey declares employment with the Department of Health and Human Services, Victoria in 2020, and is a Fellow of the Australasian Faculty of Public Health Medicine, Royal Australasian College of Physicians; Alexandra Chung declares a VicHealth postdoctoral Research Fellowship, payment for lectures (Monash University), and conference support (the Australian Prevention Partnership Centre); and Elizabeth Sturgiss declares grants (RACGP, VicHealth) and payment for lectures (East Victoria General Practice Training).
The statements or opinions expressed in this article reflect the views of the authors and do not necessarily represent the official policy of the AMA, the MJA or InSight+ unless so stated.
Subscribe to the free InSight+ weekly newsletter here. It is available to all readers, not just registered medical practitioners.
If you would like to submit an article for consideration, send a Word version to mjainsight-editor@ampco.com.au.

 more_vert
more_vert