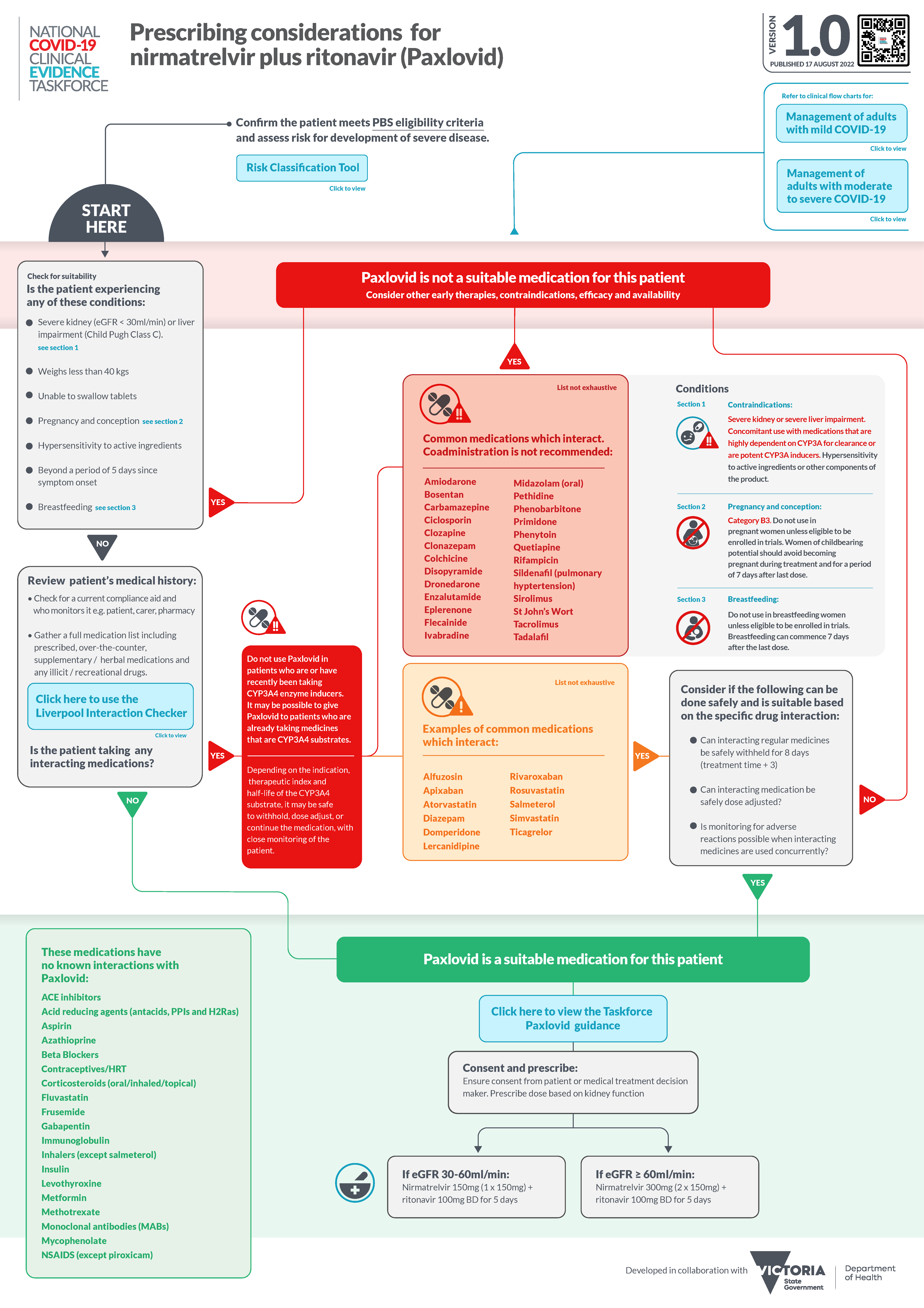
IN collaboration with the Victorian Department of Health, the National COVID-19 Clinical Evidence Taskforce has developed a Paxlovid (nirmatrelvir plus ritonavir) prescribing guide to help GPs determine its suitability for adults with mild COVID-19 and navigate the complexities of the contraindications.
The Paxlovid flow chart includes lists of medications that should not be co-administered with the antiviral, including flecainide and St John’s Wort.
For another list of medications, including rivaroxaban and three commonly used statins, depending on the specific drug interaction and suitability it suggests considering if the drug can be safely withheld for 8 days, or can be co-administered if it can be safely dose-adjusted or if close monitoring for adverse reactions is possible.
The Taskforce has also released three new flowcharts for paediatric management: Care at home for children and adolescents with mild COVID-19, Care in hospital for children and adolescents with mild to moderate COVID-19, and Care in hospital for children and adolescents with severe to critical COVID-19.
Experts react to Langya virus infections in China
A letter published recently in the New England Journal of Medicine has detailed the emergence of a new zoonotic henipavirus, Langya henipavirus (LayV) in China. The researchers identified 35 patients with acute LayV infection in the Shandong and Henan provinces of China, among whom 26 were infected with LayV only (no other pathogens were present). “These 26 patients presented with fever (100% of the patients), fatigue (54%), cough (50%), anorexia (50%), myalgia (46%), nausea (38%), headache (35%), and vomiting (35%), accompanied by abnormalities of thrombocytopenia (35%), leukopenia (54%), and impaired liver (35%) and kidney (8%) function,” they wrote. Griffith University’s Dr Xiang Liu said: “LayV is closely related to Hendra virus and the Nipah virus, which are endemic to Southeast Asia. Though the estimated fatality rate of Nipah virus is at 40% to 75%, no death has been associated with LayV infection as of today. As Hendra virus and Nipah virus are both zoonotic viruses transmitted through bats and rodents, the LayV was thought to be transmitted from animals to humans. Shrews have been suggested to be the natural reservoir for LayV. Notably, shrews are widely distributed in eastern and northeast China, some of which live in close proximity to humans. Based on the 35 clinical patients, no clear evidence has been found for human-to-human transmission, although ongoing monitoring is suggested as the transmission pattern of the virus could be altered by adaptive mutations.” Professor Eddie Holmes from the Sydney Infectious Diseases Institute said: “There is no evidence that it transmits between humans, with every case likely an independent spillover from animals. There is also no evidence for severe disease. As such, there is no particular need to worry about this virus at the moment, although ongoing surveillance is of importance.” Associate Professor Sanjaya Senanayake from the Australian National University said: “Regarding this infection, it is still early days, but there are some reassuring signs, namely that there haven’t been deaths or many serious illnesses from it, that there don’t seem to have been many cases (the earliest case seems to have been 2018), and that person-to person-transmission hasn’t been found (unlike monkeypox and COVID-19). The reason to be vigilant about this virus though is that it is a henipavirus, which comes from the same family as Hendra and Nipah, both of which have caused deaths in humans. Nipah has also been associated with person-to-person transmission.”
Time to talk with women about anal sex
Clinicians’ reluctance to discuss possible harms of anal sex is letting down a generation of young women who are unaware of the risks, warns an editorial in The BMJ. UK surgeons Tabitha Gana and Lesley Hunt wrote that as anal intercourse becomes more common among heterosexual couples, failure to discuss it “exposes women to missed diagnoses, futile treatments, and further harm arising from a lack of medical advice”. They say health care professionals, particularly those in general practice, gastroenterology, and colorectal surgery, “have a duty to acknowledge changes in society around anal sex in young women, and to meet these changes with open neutral and non-judgemental conversations to ensure that all women have the information they need to make informed choices about sex”. In Britain, the National Survey of Sexual Attitudes and Lifestyle shows participation in heterosexual anal intercourse among 16–24-year-olds rose from 12.5% to 28.5% over the past few decades. Similar trends are seen in the US, where 30–44% of men and women report having anal sex. Young women cite pleasure, curiosity, pleasing the male partners, and coercion as factors. Up to 25% of women with experience of anal sex report they have been pressured into it at least once. Anal intercourse is considered a risky sexual behaviour because of its association with alcohol, drug use, and multiple sex partners. But it is also associated with specific health concerns, explain Gana and Hunt. For example, increased rates of faecal incontinence and anal sphincter injury have been reported in women who have anal intercourse. Women are also at a higher risk of incontinence than men, due to their different anatomy. Effective management of anorectal disorders requires understanding of the underlying risk factors, and good history taking is key, they say. Yet clinicians may shy away from these discussions, influenced by society’s taboos.
Black Tuesday bushfires linked to PTSD
Research from the University of Adelaide, Flinders University and ANU, published in the Australian Journal of Rural Health, has shown people who are forced to relocate after a bushfire are at a higher risk of suffering from post-traumatic stress disorder (PTSD). Data were analysed from 179 respondents to a questionnaire who were affected by the 2005 “Black Tuesday” Eyre Peninsula bushfires, which took nine lives, destroyed 93 homes and blackened 80 000 hectares of land near Port Lincoln on 11 January 2005. Researchers contacted them at 6 months after the bushfires, with 103 and 87 participants at 2 and 7 years, respectively. The proportion of PTSD cases at times 1, 2 and 3 were 13.4% (24/179), 10.7% (11/103), and 4.8% (4/87), respectively. At 6 months, terrifying experience of fire reduced odds of developing PTSD (odds ratio [OR], 0.45; 95% CI, 0.21–0.96), whereas relocation increased odds (OR, 2.93; 95% CI, 1.06–8.08). At 2 years, relocation (OR, 6.81; 95% CI, 1.07–43.41) was a positive predictor. At 7 years, personal loss from the fires (OR, 2.82; 95% CI, 1.17–6.77) positively predicted PTSD. “People who relocate after a bushfire should be carefully assessed and supported to reduce PTSD,” said the authors. “These individuals need to be monitored over time and offered psychological support to prevent long-term psychopathology issues. Those who suffer from personal loss also need to be monitored on a long-term basis and adequately supported to compensate for the loss of loved ones. Implementing outreach programs where victims can have access to a GP or psychiatrist or psychologist will be useful for their short-term mental health. Psychological issues after a natural disaster can be delayed or manifest into something more serious if not treated early.”
Subscribe to the free InSight+ weekly newsletter here. It is available to all readers, not just registered medical practitioners.

 more_vert
more_vert