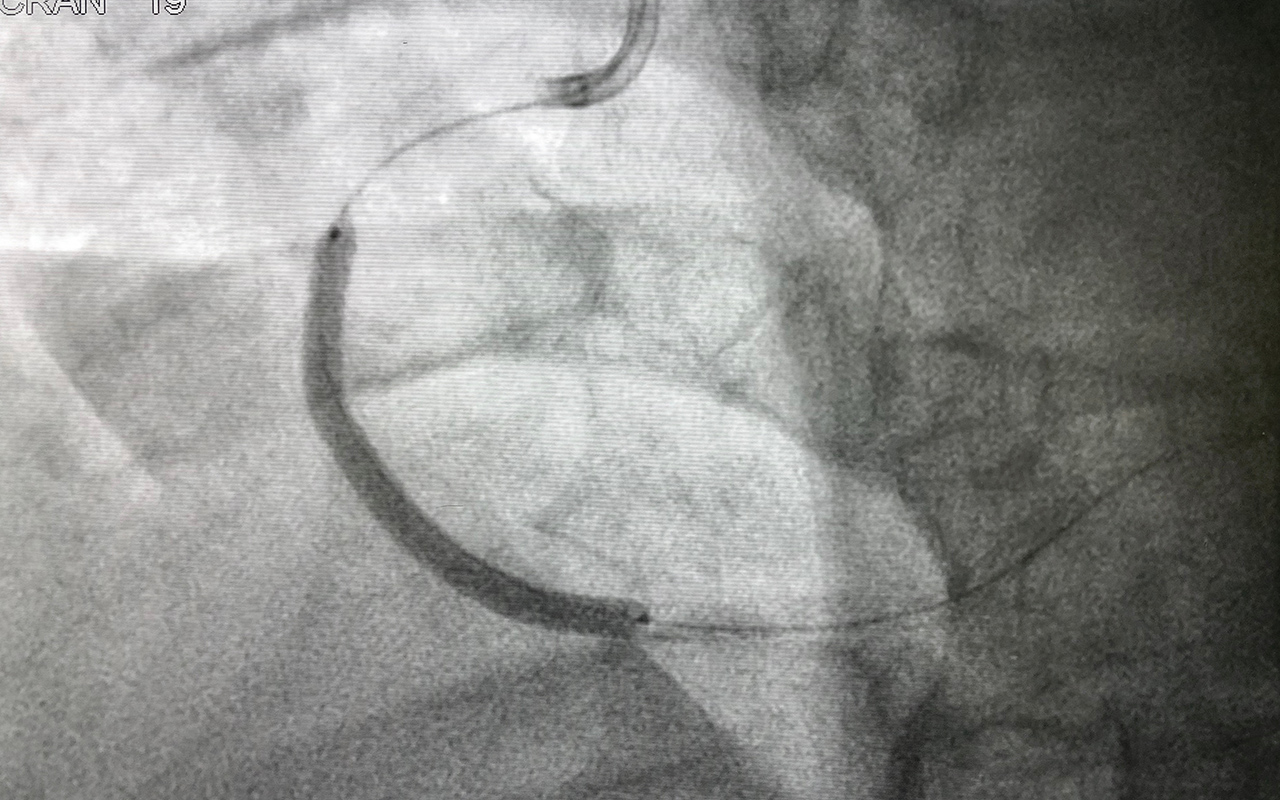
Ten percent of PCI-stent recipients miss recommended drug therapy post-discharge
TEN percent of patients undergoing percutaneous coronary intervention with stent implantation (PCI-S) for the treatment of coronary artery disease did not receive guideline-recommended dual antiplatelet therapy within 30 days of their procedure, according to the authors of a research letter published by the MJA. The authors, led by Dr Benjumin Hsu, a Research Fellow at the Centre for Big Data Research at UNSW, analysed de-identified, linked Pharmaceutical Benefits Scheme (PBS) and Medicare Benefits Schedule (MBS) data for a 10% random sample of Medicare beneficiaries, provided by the Australian Department of Health, to quantify rates of antiplatelet drug dispensing within 30 days of PCI-S. “Of 2869 patients who underwent PCI-S during the study period, 2592 (90%) were dispensed antiplatelet drugs within 30 days of the procedure,” Hsu and colleagues found. “Our findings indicate that 10% of patients undergoing PCI-S did not receive guideline-recommended dual antiplatelet therapy within 30 days of their procedure … Dispensing was more frequent for concessional PBS beneficiaries, patients who had not undergone PCI-S in the preceding year, patients not dispensed antiplatelet drugs during the preceding 6 months, and patients dispensed proton pump inhibitors within 30 days of the procedure. Antiplatelet therapy was also more frequent among patients from Victoria or Tasmania, Queensland, and Western Australia than for those from NSW or the Australian Capital Territory … Cost may have been a barrier, as antiplatelet therapy was less frequent among general than concessional PBS beneficiaries; the maximum out-of-pocket cost for any single PBS item in 2013 was $5.90 for concessional beneficiaries, but $36.10 for general beneficiaries, and general beneficiaries may have already experienced significant out-of-pocket costs for both health insurance and their procedure,” the authors wrote. “In most states, the Public Hospitals Pharmaceutical Reform Agreement ensures that PBS-subsidised medications can be dispensed to patients when they are discharged from hospital. NSW and the ACT, however, do not participate in this agreement; patients are discharged from public hospitals with unsubsidised medicines sufficient for only 2–7 days, after which they must visit a community doctor for prescribing of PBS-subsidised medications. This inconvenience may contribute to the lower 30-day dispensing rate in these jurisdictions.” The authors recommended that further research be undertaken to investigate why some patients undergoing PCI-S are not receiving dual antiplatelet therapy directly after their procedure.
Fish oil supplements may improve heart health
Regular use of fish oil supplements may be linked to a lower risk of death and cardiovascular disease (CVD) events, such as heart attack and stroke, suggests an analysis of data from the UK Biobank study, published in The BMJ. The researchers’ analysis included 427 678 men and women aged between 40 and 69 years, without CVD or cancer, who were enrolled in the study from 2006 to 2010 and completed a questionnaire on supplement use, including fish oil. Death certificates and hospital records were used to monitor all-cause mortality, CVD deaths, and CVD events, such as heart attack and stroke, through to 2018. Almost a third (31%) of participants reported taking regular fish oil supplements at the start of the study. The researchers found that fish oil supplements were associated with a 13% lower risk of all-cause mortality, a 16% lower risk of CVD mortality, and a 7% lower risk of CVD events (388 fewer all-cause deaths, 124 fewer CVD deaths, and 295 fewer CVD events per 100 000 people in a median follow-up of 9 years). The association between fish oil use and CVD events appeared to be stronger among individuals with high blood pressure. These favourable associations remained after taking account of traditional risk factors, such as age, sex, lifestyle habits, diet, medication and other supplement use. Results were also unchanged after further analyses, suggesting that the findings withstand scrutiny. Several mechanisms could explain these results, say the researchers. For example, omega-3 fatty acid supplements have shown beneficial effects on blood pressure, cholesterol levels, and heart rate, all of which would exert a protective effect against the development of CVD events. Despite the large sample size, this is an observational study, so it can’t establish cause, and the researchers point to some limitations, such as lack of information on dose, duration, and side effects of fish oil use.
Moderate egg intake not associated with cardiovascular disease risk
A study published by The BMJ adds to evidence that moderate egg consumption (up to one egg per day) is not associated with cardiovascular disease (CVD) risk. To evaluate the association between egg intake and CVD, repeated measures of diet and lifestyle factors over a long period of time are needed. It is also important to consider the effect of eggs on CVD risk compared with other animal and plant-based foods. US researchers investigated the link between egg intake and cases of CVD – including non-fatal heart attack, fatal coronary heart disease, and stroke – using repeated measures of diet over a period of up to 32 years, starting from 1980. Their findings are based on data from three large US cohort studies: the Nurses’ Health Study (NHS), the NHS II, and the Health Professionals’ Follow-Up Study (HPFS). These included 83 349 female nurses aged 30–55 years, 90 214 female nurses aged 25–44 years, and 42 055 male health professionals aged 40–75 years respectively, who were free of CVD, type 2 diabetes, and cancer at the start of the study. During the follow-up period, there were 14 806 cases of CVD, including 9010 cases of coronary heart disease and 5903 cases of stroke. Most people ate between one to five eggs per week, and those with a higher egg intake had a higher body mass index, were less likely to be treated with statins, and ate more red meat. After adjusting for age, lifestyle, and dietary factors, no association was found between egg intake and risk of CVD. There was an estimated higher risk of CVD when the researchers statistically replaced one whole egg a day with one serving of processed red meat (15%), unprocessed meat (10%) or full fat milk (11%), but foods such as fish, poultry, legumes, cheese and nuts in place of eggs were not linked to CVD risk. Results from an updated meta-analysis of 28 observational studies further support the overall lack of an association between egg intake and CVD risk, but evidence varied between studies conducted in the US, Europe and Asia. There was no overall association between egg intake and CVD risk among US and European studies, but moderate egg consumption was associated with a slightly lower CVD risk in Asian populations. This is potentially explained by the fact that in Asian cultures, eggs are typically included in a variety of different dishes, while in Western populations, eggs tend to be eaten with red and processed meats and refined grains. This is an observational study, and as such, can’t establish cause. And the authors point to some limitations, including that the three cohorts were made up of health professionals and, therefore, the findings may not be reflective of the general population.
What’s new online at the MJA
Perspective: An outbreak of COVID-19 caused by a new coronavirus: what we know so far
Cheng and Williamson; doi: 10.5694/mja2.50530
Information on COVID-19 and its impact is being updated constantly and Australia must continue to be prepared at all levels of the health care system … FREE ACCESS for one week
Podcast: Professor Allen Cheng, Director of the Infection Prevention and Healthcare Epidemiology Unit at Alfred Health, talking about coronavirus … OPEN ACCESS permanently
Perspective: Breathing life into Australian diabetes clinical guidelines
White et al; doi: 10.5694/mja2.50509
Living guidelines that incorporate new evidence as it becomes available have the potential to overcome some of the limitations inherent in static guidelines … FREE ACCESS for one week
Research letter: Antiplatelet therapy within 30 days of percutaneous coronary intervention with stent implantation
Hsu et al; doi: 10.5694/mja2.50507
Why some patients are not receiving dual antiplatelet therapy after their procedure should be further investigated … OPEN ACCESS permanently
Research letter: Isolation and rapid sharing of the 2019 novel coronavirus (SAR-CoV-2) from the first diagnosis of COVID-19 in Australia
Lewin et al; Pre-print rapid access … OPEN ACCESS permanently
Research: Impact of corticosteroid treatment in patients with coronavirus disease 2019
Zha et al; Pre-print rapid access … OPEN ACCESS permanently

 more_vert
more_vert