Assisted dying not driven by poverty or poor access to health care
A Canadian study of people who received voluntary assisted dying (VAD) – known as medical assistance in dying in Canada – in Ontario found that about three-quarters were cared for by palliative care practitioners at the time of their request for VAD, and VAD recipients were younger, wealthier and more likely to be married than the general population at time of death. These findings dispel concerns that VAD requests are driven by lack of access to palliative care services or by socio-economic vulnerabilities. The study was published in CMAJ along with a related editorial. VAD was legalised in Canada in June 2016, and as of October 2018, 6749 Canadians had received VAD. The federal government and the Government of Quebec are currently in consultation around drafting new eligibility criteria for VAD, after a decision of the Quebec Superior Court that one provision of the previous laws violated the Canadian Charter of Rights and Freedoms. Researchers analysed clinical and socio-economic data from 2241 Ontarians who received VAD, and compared this with data from all 186 814 people in the province who died between June 2016 and October 2018, from databases kept by the Office of the Chief Coroner for Ontario and ICES. Among patients who received VAD, the median age was 75 years and half were women; almost two-thirds of patients (64%) had cancer, 12% of patients had neurodegenerative disease, 8.5% had cardiovascular disease and 7.5% had respiratory disease. Patients who received VAD reported both physical (99.5%) and psychological (96.4%) suffering. The study found that only 6.6% of families reported challenges with access to VAD and these delays were not associated with socio-economic status. The authors noted, however, that the VAD dataset included only people who actually received VAD, so these findings would not reflect the experience of patients who requested VAD but never received it.
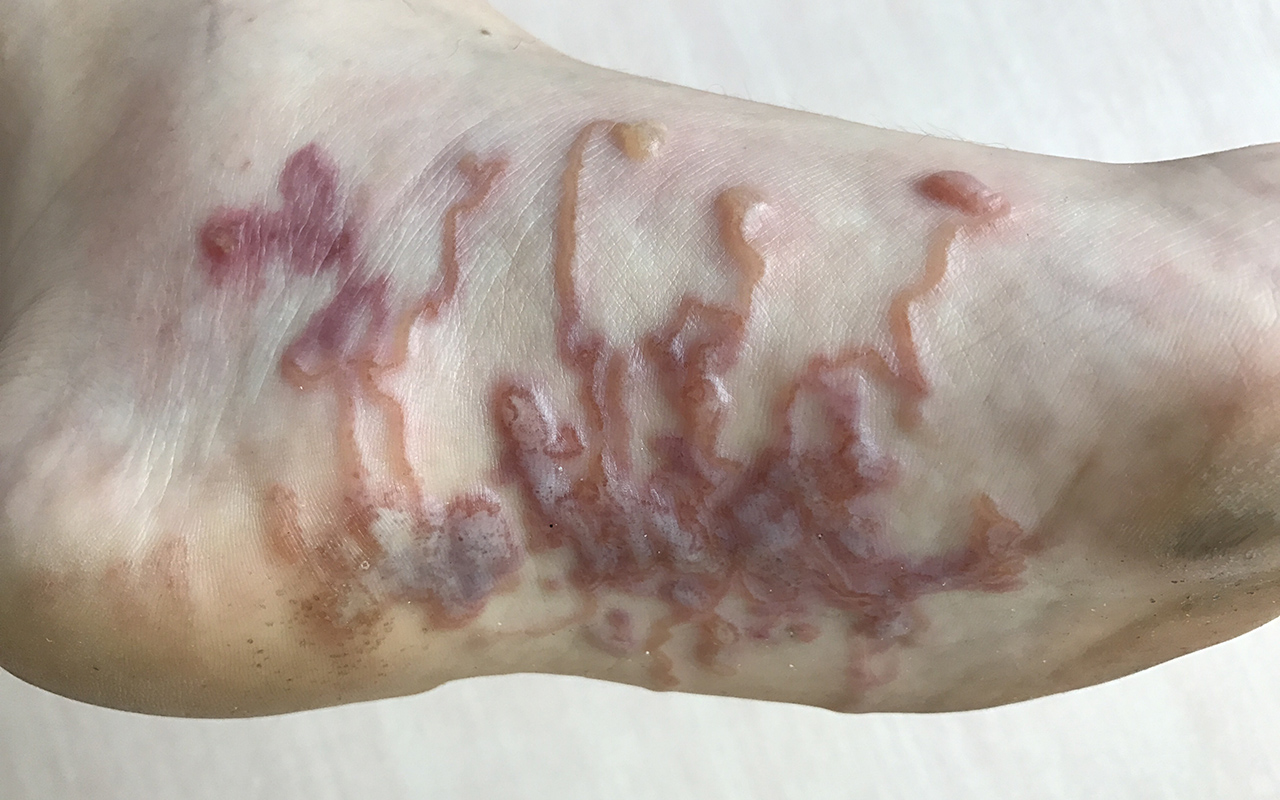
Cracking the code for hookworm infestation
Monash University researchers have uncovered a key way that hookworms evade the immune system, providing new hope in the search for a vaccine. Importantly, the researchers, led by Professor Nicola Harris from Monash University’s Central Clinical School, may have discovered why people are unable to kill these parasites. Hookworms infect nearly around 700 million people in the world, mostly in countries where sanitation is poor, and people often walk barefoot. The body’s immune system is critical to attacking the hookworm, but these parasites are masters of escape and individuals typically remain infected throughout their lifetime, often resulting in death or complications stemming from anaemia. The research, published in Cell Host and Microbe, shows that a type of immune cell in the blood, neutrophils, can kill hookworms by releasing neutrophil extracellular traps (NETs) made up of toxin-coated DNA. However, the hookworm has developed a way to sense what the neutrophil is doing, releasing an enzyme that degrades the DNA backbone of the trap, allowing the hookworm to remain and continue infecting its host. Professor Harris and her colleagues suggest the NETs created by the neutrophils could kill the worm, providing people living in hookworm-prone areas by boosting much needed immunity. Professor Harris says that the discovery could form the basis of a vaccine to achieve this goal. “We may now be able to look at new vaccination approaches that target the enzyme secreted by the hookworm parasite to alleviate infestation and to decrease the likelihood of re-infection.”
Pinpointing rogue cells at root of autoimmune disease
For the first time, a team led by researchers at the Garvan Institute of Medical Research have pinpointed individual cells that cause autoimmune disease from patient samples. They also uncovered how these cells “go rogue” by evading checkpoints that normally stop immune cells from targeting the body’s own tissues. The findings were published in Cell. There are more than 100 different autoimmune diseases, but what unites them all is that they arise from an individual’s own cells – rare and mysterious immune cells that target not external viruses and bacteria but the body’s own healthy organs and tissues. By first separating individual cells, and then separating their genetic material, the researchers isolated immune cells that produced rheumatoid factors – antibody proteins that target healthy tissues in the body and are associated with the most common autoimmune diseases, including rheumatoid arthritis. Once isolated, the researchers then analysed the DNA and messenger RNA of each of these rogue cells, scanning more than a million positions in the genome to identify DNA variants that may be at the root of disease. They found that the disease-causing immune cells of the patients with vasculitis had accumulated a number of mutations before they produced the damaging rheumatoid factors. The researchers found that some of the first gene mutations that occurred in these rogue cells were known to drive lymphomas. Further, the researchers found that cells with the lymphoma driver mutations accumulated further mutations that caused the rheumatoid factors they produced to aggregate, or “clump together”, at lower temperatures. The researchers are now planning follow-up studies to investigate mutations of autoimmune cells in a range of other diseases, including lupus, coeliac disease and type 1 diabetes.
What’s new online at the MJA
Podcast: Associate Professor Danny Youlden is the Senior Manager of Childhood Cancer Research at Cancer Council Queensland. He discusses the incidence of childhood cancers in Australia … OPEN ACCESS permanently
Perspective: Setting the record straight: sexually transmitted infections and sexual abuse in Aboriginal and Torres Strait Islander communities
Ward et al; doi: 10.5694/mja2.50492
The automatic assumption that sexually transmissible infections in young people means sexual abuse further stigmatises them and discourages them from presenting to health services … OPEN ACCESS permanently
Research letter: Validating Indigenous status in a regional Queensland hospital emergency department dataset with patient-linked data
O’Loughlin et al; doi: 10.5694/mja2.50401
Inaccurate recording of Indigenous status in administrative datasets can influence health service decision making … OPEN ACCESS permanently

 more_vert
more_vert