DOCTORS must get their “house in order” when talking about sepsis, says a leading infectious diseases physician who is supporting calls for a national plan to reduce preventable deaths and disability from the condition.
Professor David Paterson, consultant infectious diseases physician and Director of the University of Queensland Centre for Clinical Research, said the term “sepsis” was often incorrectly used in many medical specialties.
“When I talk to an orthopaedic surgeon, for example, they may talk about a patient having sepsis, and what they are referring to is a person having an infection in their joint or in their wound, which is a very different thing from what an intensive care unit (ICU) or emergency doctor would talk about with sepsis,” said Professor Paterson.
“There are some situations where people equate an infection in your blood with sepsis, and again, that’s not correct.”
In the MJA, experts have called for a nationwide plan to better identify and manage sepsis, which was defined as “life-threatening organ dysfunction due to a dysregulated host response to infection”.
The call comes in the wake of a 2017 World Health Organization resolution on sepsis urging member states to take specific actions to reduce the burden of the condition, which was a “leading but poorly recognised case of death and disability”. The resolution was cosponsored by Australia.
According to estimates cited in the MJA, there were 18 000 episodes of sepsis annually in Australia, and at least 5000 deaths, which disproportionately affected the very young, the very old and Aboriginal and Torres Strait Islander people.
The MJA authors noted that capturing data on sepsis was challenging because hospital coding significantly undercounted the burden of disease. But, they added, the development of electronic medical records may improve the capacity to identify sepsis in real time and more accurately assess its incidence.
Professor Paterson said education was needed to ensure that clinicians were correctly identifying sepsis.
“Doctors have got to get their house in order first in terms of the way we use the terminology of sepsis. An ICU doctor will use [the term] correctly, but many of our colleagues probably need education about what sepsis truly is. We need to all be on the same page when we are communicating with each other, and also when we are communicating with patients and the community in general.”
Professor Simon Finfer, co-author of the MJA article and Director of the Australian Sepsis Network, said Australia, like many countries around the world, had a problem with the identification and early management of sepsis.
“Sepsis is a whole-of-health care-system issue,” said Professor Finfer who is also Professorial Fellow in the Critical Care Division at the George Institute for Global Health. “Sepsis doesn’t have a natural advocate because it’s distributed throughout all hospital departments and specialties. We established the Australian Sepsis Network [which is hosted by the George Institute] a few years ago to try to get a coordinated response to sepsis and to improve treatment.”
Professor Rinaldo Bellomo, Professor of Intensive Care Medicine at the University of Melbourne, said the broad nature of sepsis made improving identification and awareness challenging.
“Sepsis happens everywhere, it can happen in cancer patients, in people in the community developing pneumonia, it can happen in the Indigenous community from a scratch in the leg becoming infected, it can happen in neonates, it can happen in a child developing meningococcal bacteraemia and dying,” he said. “It’s not segmented and siloed in a neat, tidy way that allows easy focusing and easy explanation to the public.”
Professor Finfer said the Australian Sepsis Network regularly fielded queries from people who had experienced adverse impacts of sepsis. He said the two most common contacts were from people who had had a delayed diagnosis resulting in severe disability or the death of a loved one, and from people who had recovered from sepsis but developed one of the common long term sequelae, which were cognitive, physical or psychological impacts.
“These can severely impact their life and are grossly under-recognised within the medical community, so there are no services for these people,” Professor Finfer said.
Community awareness of sepsis was very low, he said, pointing to a 2016 survey conducted by the Australian Sepsis Network and the George Institute for Global Health that found that six in ten Australians had never heard of sepsis.
“We found that 40% of Australians had heard of sepsis and that was much more common in the elderly population, probably because they either had had sepsis or someone they knew had had it. And after they had been told what sepsis was, only 14% of people thought that fever and shivering could be a sign of sepsis,” he said, noting that only 1% of respondents knew that rapid breathing, rapid heart rate and confusion could be signs of sepsis.
“There is an issue not just with the term sepsis but with people understanding when they should seek urgent medical attention.”
Professor Finfer said public awareness campaigns in the UK, Germany and parts of the US had been successful in alerting communities of the signs and symptoms of sepsis.
He said such a campaign was part of a four-point national plan proposed by the Australian Sepsis Network and the George Institute. The plan includes:
- a nationally coordinated sepsis body to develop and promulgate a national action plan;
- a prevention and awareness campaign targeting the community and the health care workforce;
- nationally recognised clinical standards for the detection and treatment of sepsis; and
- investment in community and peer support services for sepsis survivors and their families.
Several states have initiated programs to tackle sepsis in the hospital environment – including the Sepsis Kills program in New South Wales, Queensland’s Sepsis Breakthrough Collaborative, and Victoria’s Think Sepsis: Act Fast collaboration – but, Professor Finfer said, the best solution for all Australians was a national approach.
“We are working with all federal governments and with the [Australian Commission on Safety and Quality in Health Care] to explore how we can best enact the measures that we think are important to improve sepsis outcomes. And, ultimately, that would constitute, we hope, a national action plan,” Professor Finfer said.
It’s a move supported by Professor Bellomo.
“In the hospital environment, where obviously sepsis is a big deal, there have been quite a few initiatives from state governments,” he said. “But in the community environment, where the majority of sepsis starts, it really needs to be addressed at a federal level. There has to be a media campaign, an education campaign and a GP educational campaign to begin with.”
Professor Paterson said a key element of a national plan should aim to address the rate of sepsis among Indigenous Australians.
The MJA authors highlighted a 2016 systematic review that found that the highest published incidence of sepsis in the world was among Aboriginal and Torres Strait Islander adults living in the Northern Territory.
“Australian Indigenous populations really need some special attention,” Professor Paterson said. “And without a national action plan we are going to have difficulty getting across jurisdictions to achieve improved outcomes in Indigenous populations.”

 more_vert
more_vert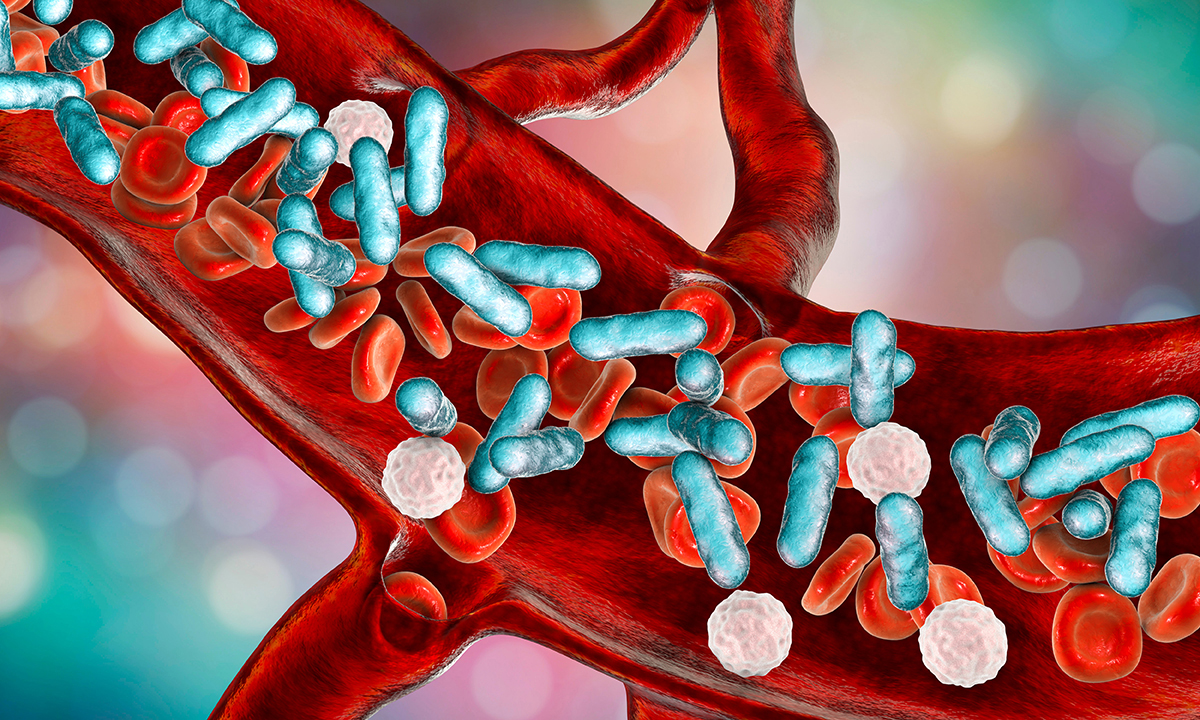
I would could be “sepsis” so treat it as such and you will save more lives.
I’d call it “severe infection” – then there is no ambiguity among doctors and there’d be good community awareness to build on for an education campaign.
I concur with the earlier correspondents. Just because you redefine an older term in a highly specific way (yes – Wikipedia will reproduce the definition you are using), doesn’t mean that people and Medicos outside your subspecialised area will understand it the way that you do. I am thus not surprised by your Orthopaedic colleague using the term for joint sepsis as an example, nor would I be surprised if the diagnoses respiratory sepsis or urosepsis appeared in a discharge summary in 2019.
The history of the word Sepsis makes it a poor choice as a precise descriptor because it has older, less precise meanings.
The word ‘sepsis’ has been around since the Ancient Greeks, the generic term to mean ‘infection’. It and its derivatives are widely known in the community, with the humble septic tank, and the plethora of antiseptic liquids/wipes in so many households.
My cohort of medical students was taught the term ‘septic shock’ to denote the type of circulatory and poly-organ failure the authors describe with the bland generic term ‘sepsis’. Their definition would confusingly call an oncology patient with no leukocytes “not septic” while he is dying of septicaemia, with no host response. Surgical “aseptic” technique would be a thing of the past. The cardiac patient whose subacute endocarditis killed him with valve rupture would be an “aseptic” death from fatal infection.
Unless we are to charge the manufacturers of Betadine Antiseptic Liquid (as used in hospitals) with false advertising, perhaps Prof Paterson is the one emulating the Queen of Hearts and is the one who is not correct. This is a case for XKCD’s Etymology Man!
Thanks for interesting insight. Historically, use of the word “sepsis” has had similar vague associations in RSA. We have “septic drains” and “septic tanks” but “septic people”?? The exception has always been the new born infant. “Sepsis Neonatorum” has historically stood the test of time. Probably because neonates have such poor ability to localise their infection to one organ and that infections are often life-threatening and immune function poor.
Thanks for an always interesting journal!
Paediatrician, Johannesburg.
Why call it sepsis?
It’s multiple organ failure , irrespective of the cause. So why not call it that, and there won’t be confusion with septicaemia
Obviously needs intensive care,and is an emergency, unlike septicaemia
I understand and appreciate the sentiment, but the word existed and had meaning not limited to host dysregulation before recent redefinitions.
This is unfortunate, but don’t blame the clinicians because you redefined a word they already used!
I have been puzzled that the very non specific term “sepsis” has crept into medical vocabulary and also is now appearing in popular culture. We used to refer to “overwhelming sepsis” , “septicaemia” and most recently SIRS, and I find the term ‘sepsis’ inadequate in denoting overwhelming infection with hyper immune responses leading to multi organ failure. I think a better and more specific descriptor is required, hopefully leading to more clarity and less confusion as to what it actually is, as has been highlighted by Prof Paterson.