THE language we use to ask about and describe health, illness, and social and emotional wellbeing is important. Hearing descriptions of symptoms and noticing signs of mental illness are our only way to make a diagnosis. Without the luxury of objective diagnostic tests for mental illness, it is essential that when we ask people to describe their mood, interests, thoughts and behaviour, we ask them in a culturally appropriate way.
Diagnosing depression, other mental illnesses or psychological distress, is not always easy in general practice. Many people with depression (~ 66%) will present to their primary care clinician with a somatic complaint rather than announcing that they have depression or anxiety. The primary care clinician needs to maintain a high index of suspicion of underlying depression or anxiety. This is likely why Murtagh refers to depressive illness as “probably the greatest masquerade in general practice”.
In Australia, studies have confirmed that commonly used tools such as the K10 and the nine-item Patient Health Questionnaire (PHQ-9) do not use language that is culturally aligned with Aboriginal and Torres Strait Islander peoples. While there are culturally adapted and new tools to screen for social and emotional wellbeing in Aboriginal and Torres Strait Islander Australians, none of the freely available tools have been validated for use outside of the community in which they were developed. Therefore, there has been a clear need to validate a tool for use with Australia’s First Nations peoples.
In our recent Getting it Right study with 500 Aboriginal and Torres Strait Islander peoples across Australia we have shown that the culturally adapted PHQ-9 (aPHQ-9) (available for download here) is culturally appropriate and valid to use to screen for depression by and with Australia’s First Nations peoples.
The aPHQ-9 contains culturally appropriate questions developed in conjunction with Aboriginal communities and researchers. The questions ask about mood, sleep, energy for activity, appetite, cognitions and impulse control. Where the original PHQ-9 questionnaire asks:
Over the past 2 weeks, how often have you been bothered by any of the following problems:
- little interest or pleasure in doing things?
- feeling down, depressed or hopeless.
The adapted (aPHQ-9) tool instead asks, over the past 2 weeks:
- have you been feeling slack, not wanted to do anything?
- have you been feeling unhappy, depressed, really no good, that your spirit was sad?
In the Getting it Right study, Aboriginal and Torres Strait Islander people attending one of ten primary health care services located in six states and territories, first completed the aPHQ-9. Participants could complete the aPHQ-9 by themselves on paper, on a computer, questions could be read out by a trained interviewer who was permitted to translate the questions into “language” or ask them using the plain English wording. Participants then completed a structured psychiatric interview conducted by a different trained interviewer who did not know the aPHQ-9 results. When the results of both interviews were compared, the aPHQ-9 reliably identified those who needed further assessment of their mood and was able to identify those who were unlikely to have depression. The sensitivity of the aPHQ‐9 algorithm for diagnosing a current major depressive episode was 54% (95% CI, 40–68%), and its specificity was 91% (95% CI, 88–94%), with a positive predictive value of 64%.
Primary care clinicians should consider using the aPHQ-9 where depression is suspected during their consultations with Aboriginal and Torres Strait Islander peoples. While screening for depression is not universally recommended, screening may be appropriate for people considered to be at high risk (see National guide box 4), when there is access to appropriate therapy and support if depression is detected.
The social and emotional wellbeing and mental health of Aboriginal and Torres Strait Islander peoples are national health priorities. Regular use of the aPHQ-9 by culturally competent clinicians who are confident that appropriate support and treatment is available may help to facilitate the delivery of equal, accessible, sustainable, timely and culturally competent primary health care that respects and promotes cultural integrity.
The aPHQ-9 should be easily accessible by all primary care clinicians. In addition to incorporating the aPHQ-9 in the Medicare Health Assessment for Aboriginal and Torres Strait Islander People (Medicare Benefits Schedule item 715), it should also be made available in all general clinical and practice management software for those clinicians who see Aboriginal and Torres Strait Islander peoples.
Before the aPHQ-9 was validated for use across Australia, primary care doctors working with Aboriginal and Torres Strait Islander peoples often used screening tools not fit for purpose to help manage an area of health of paramount importance to all Australians. The aPHQ-9 is a welcome addition to the GP toolbox.
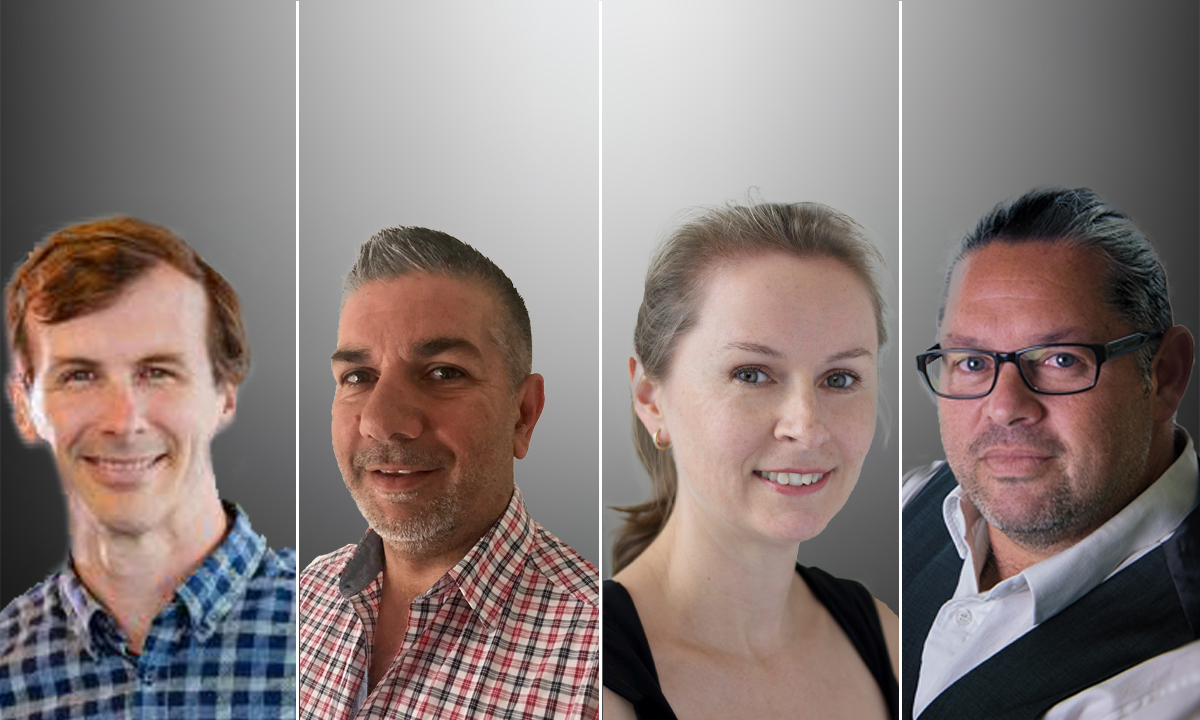
Dr Geoff Spurling is a Senior lecturer in the Discipline of General Practice at the University of Queensland.
Dr Jamie Fernando is at the Glen Centre, in New South Wales.
Professor Maree Hackett is from the George Institute for Global Health, at the University of New South Wales.
Professor Alex Brown is from the South Australian Health and Medical Research Institute, and the University of South Australia.
The statements or opinions expressed in this article reflect the views of the authors and do not represent the official policy of the AMA, the MJA or InSight+ unless so stated.

 more_vert
more_vert