LEVONORGESTREL-releasing intrauterine devices (LNG-IUDs) are playing a growing role in the management of heavy menstrual bleeding in Australian women accepting of hormonal management options, say experts in the MJA this week.
In a Narrative Review, Dr Annabelle Brennan and Professor Martha Hickey of Melbourne’s Royal Women’s Hospital outlined the current medical and surgical approaches to two of the most common causes of menstrual disturbance: endometrial dysfunction and leiomyomas (or fibroids).
Dr Brennan said that abnormal uterine bleeding – encompassing change in regularity, frequency, heaviness or length of menstruation – could have a significant effect on women of all ages.
“It’s not just the need to take time off work, but having to take a change of clothes, worrying about staining, and missing out on social activities because the bleeding really interferes with their life,” she told MJA InSight.
Dr Brennan said that about 70% of women aged 50 years and over had fibroids, although not all of these women would be symptomatic; and about one third of women would experience abnormal bleeding associated with primary endometrial dysfunction.
She said that there was a huge range of options for managing abnormal uterine bleeding, with advantages and disadvantages to each approach.
“This review allows clinicians and their patients to be better informed about the management options available,” Dr Brennan said.
“Each patient has different needs, and every patient experiences abnormal menstruation in their own way. It’s important to understand the patient that you have in front of you and their particular issues, then you can come to a decision about which management option is going to be the right choice for them at their current stage of life, and that may change over time.”
The review noted that for heavy menstrual bleeding associated with primary endometrial dysfunction, LNG-IUDs were considered first-line medical management in women accepting of hormonal therapies. Alternative medical approaches included tranexamic acid, non-steroidal anti-inflammatory drugs, the combined oral contraceptive pill and oral progestins, the authors wrote.
They said that the number of IUDs inserted for heavy menstrual bleeding had quadrupled over the past decade. Medicare data showed that more than 3300 IUD insertions in 2016 were for heavy menstrual bleeding, representing an increase from 3% to 5% of total IUD insertions over the previous decade.
Dr Brennan said that the review highlighted the advantages of LNG-IUDs for women wanting to preserve their fertility. She said that the increasing use of LNG-IUDs for heavy blood loss was likely to continue as clinicians and patients became more familiar with the advantages of this approach.
“Our research has shown that [LNG-IUDs] are reducing blood loss by well over 90%, and more than half of all women who have an IUD will end up having no blood loss at all, which is a very effective form of treating bleeding disturbance,” Dr Brennan said.
“LNG-IUDs offer a wonderful solution that is very effective, quickly reversible and cost-effective.”
Dr Elizabeth Farrell, Medical Director of Jean Hailes for Women’s Health, welcomed the review.
She said that the introduction of the LNG-IUD had been a significant advance in helping women with heavy menstrual bleeding.
“It has helped to reduce rates of hysterectomy, which may have been carried out more in younger women because there didn’t seem to be an alternative,” Dr Farrell told MJA InSight.
While she said that the LNG-IUD was not the “be-all-and-end-all” for every woman, it played multiple roles in managing menstrual disruption.
“There is no other therapy that reduces blood flow by 95%, apart from surgery. It can be removed, it retains fertility, and it can be used in the peri-menopause,” Dr Farrell said. “We can also use it as a progestin in those women who require hormone therapy in the peri-menopause and the early post-menopause, and it can be used for menstrual pain as well as heavy bleeding.”
Dr Farrell also highlighted the role of tranexamic acid, particularly while investigating the causes of abnormal uterine bleeding.
“Tranexamic acid is something I would use as a first-line therapy while we are doing investigations to see if we can find a cause,” she said. “It only needs to be used on the heavy days of the period and reduces blood flow by 56%. It is widely used as a first-line treatment in Scandinavia, but many GPs don’t include it in their choice of therapies.”
The review said that hysterectomy was the “definitive surgical approach” for abnormal uterine bleeding and was associated with high levels of patient satisfaction (up to 90%). For patients wanting to preserve their fertility, they said, myomectomy was an option for women with symptomatic fibroids.
The authors noted that several minimally invasive surgical management options were also available – including uterine artery embolisation and magnetic resonance-guided focused ultrasound surgery.
“There is increasing use of these minimally invasive procedures,” Dr Brennan said, noting that research was under way to determine the effects of these techniques on fertility.
To find a doctor, or a job, to use GP Desktop and Doctors Health, book and track your CPD, and buy textbooks and guidelines, visit doctorportal.

 more_vert
more_vert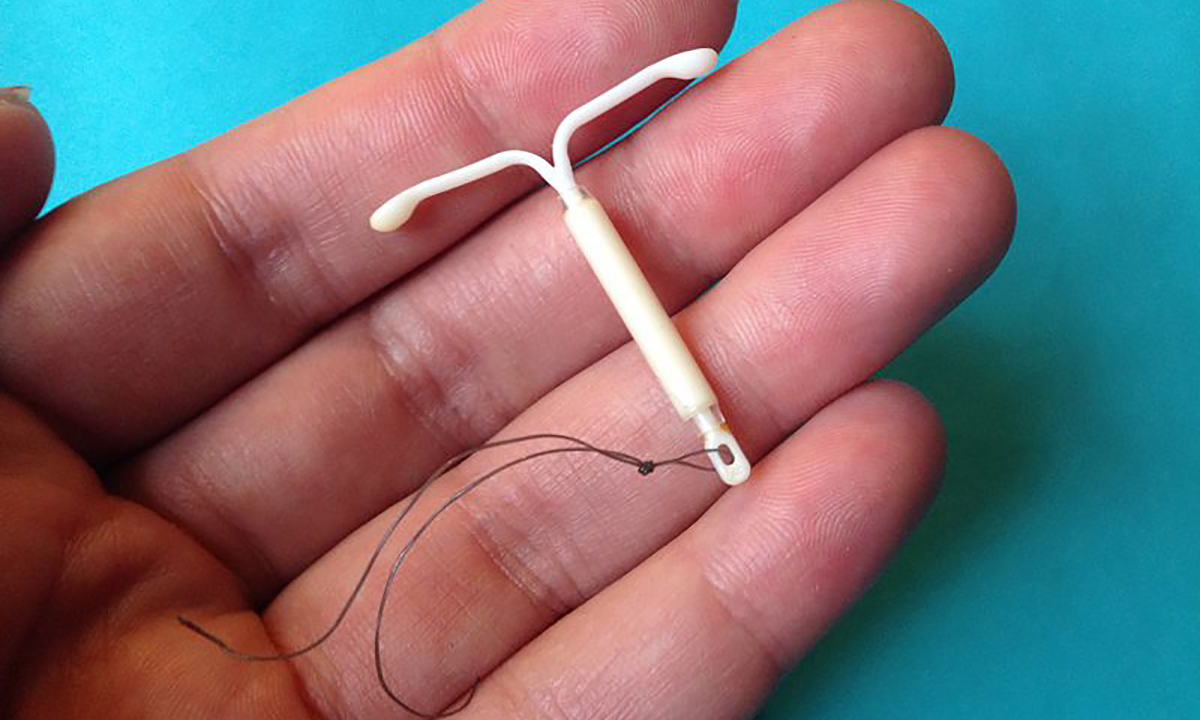
irregular bleeding in young girls is often eliminated by talking to them to change taking pill around lunch or tea time
for regularity.
most like to , when they get up or before going to sleep. and either can be irregular,easy to forget specially in young working girls while they are more prone to infections due to presence of string and change in partners and so on.