ONCE neglected by researchers and underdiagnosed in practice, there is renewed interest in the chronic lung disease bronchiectasis, according to the authors of a Narrative Review of the condition, published in the MJA.
Bronchiectasis is characterised by chronic cough, sputum production and recurrent pulmonary exacerbations. It is diagnosed radiologically on high resolution computed tomography chest scan by bronchial dilatation. A large proportion of cases are of unknown cause, reflecting the incomplete understanding of the disease.
Dr Simone Visser, a respiratory physician at Royal Prince Alfred Hospital (RPA), Professor Peter Bye, from the University of Sydney and RPA, and Associate Professor Lucy Morgan, a senior respiratory physician at Concord Repatriation General Hospital in Sydney, wrote that the prevalence of bronchiectasis was increasing worldwide, but the burden of disease within Australia was not well defined.
That led to the establishment of the Australian Bronchiectasis Registry in 2016.
“Recent prevalence estimates in the United Kingdom [are] 566 per 100 000 women and 485 per 100 000 men,” Visser and colleagues wrote.
“Females, the elderly, and Indigenous populations are more frequently affected. Notably, Indigenous children in Australia’s Northern Territory have an extremely high disease prevalence of 14.7 per 1000 children.
“The economic burden of bronchiectasis is significant; a recent study conducted in New Zealand reported an annual hospitalisation cost of NZD$5.34 million. Quality of life impairment in patients with bronchiectasis is equivalent to the impairment seen in patients with severe chronic obstructive pulmonary disease (COPD).”
Frontline management of bronchiectasis remains airway clearance on a daily basis.
“All patients should be referred to a specialised respiratory physiotherapist, who can personalise an airway clearance regimen. This may include a combination of aerobic exercise, active cycle of breathing, positive expiratory pressure devices and postural drainage,” wrote Visser and colleagues.
Other recommendations from the authors included:
- antibiotics should be used in a timely manner for pulmonary exacerbations (worsening of symptoms from the patient’s normal baseline) and targeted to the patient’s previous sputum pathogens;
- long term use of oral macrolide antibiotics in selected patients to reduce exacerbation frequency;
- the routine use of long term inhaled corticosteroids and/or long-acting bronchodilators should be avoided, unless concomitant COPD or asthma exists;
- the evidence for nebulised agents including hypertonic saline, mannitol and antibiotics is evolving; however, access is challenging outside tertiary clinics, and nebulising equipment is required;
- smokers should be supported to quit;
- all patients should receive influenza and pneumococcal vaccination;
- patients with impaired exercise capacity should attend pulmonary rehabilitation; and
- there is an important minority of patients for whom aetiology-specific treatment exists.
“Data from the Australian Bronchiectasis Registry and the addition of an Australian Refined Diagnostic Related Group bronchiectasis code will provide insight into the burden of disease and patterns of care in Australia,” Visser and colleagues concluded.
To find a doctor, or a job, to use GP Desktop and Doctors Health, book and track your CPD, and buy textbooks and guidelines, visit doctorportal.

 more_vert
more_vert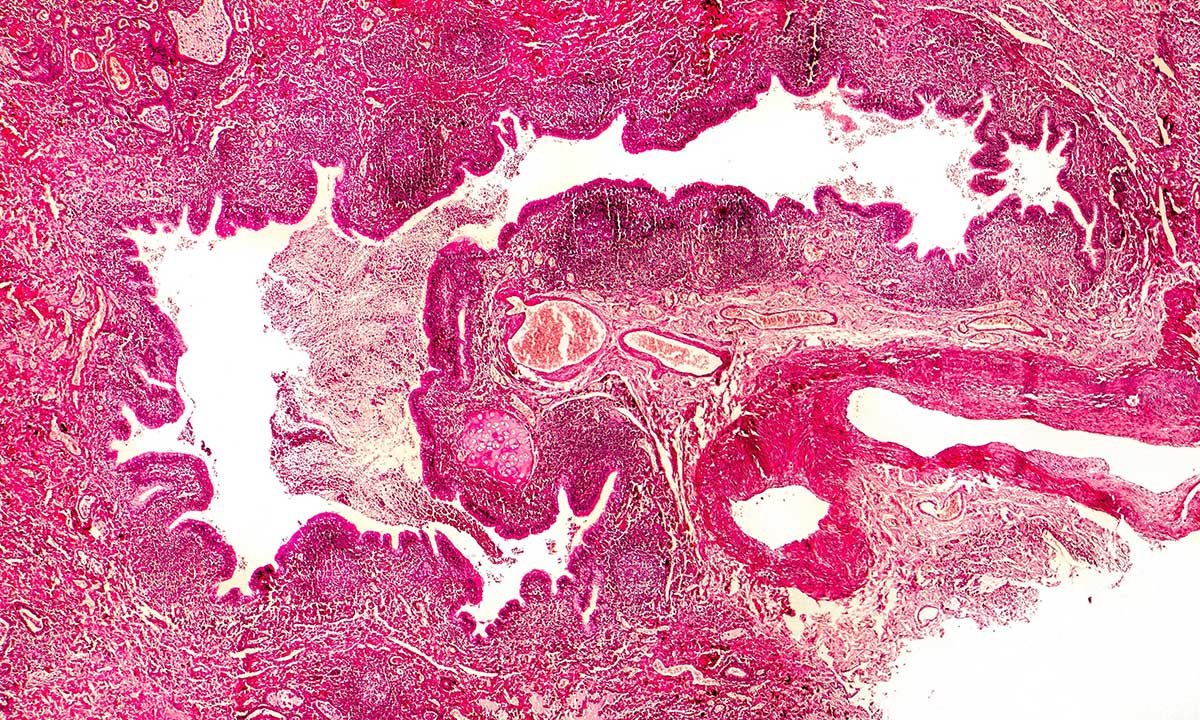
Very useful information.
Any chance of free respiratory physio exercises or centres to attend?
Am currently not working.
Am seeing Dr Visser next week.