SIMILAR to many other facets of our lives, the delivery of health care is undergoing a period of rapid digital change. The advent of innovative new technologies in health care, including mobile applications, wearable devices and artificial intelligence, has entered mainstream discourse, and health care is often described as the last frontier of “disruption”. Indeed, given time, these technologies have promise in empowering patients and transforming the way we prevent, diagnose and manage disease – fundamentally changing the clinician–patient relationship.
Digital health innovation has a checkered history in delivery. As we enter this period of transformation, we believe that clinicians should be at the forefront of this change. Clinicians, working with other stakeholders, are best placed to ensure that future innovations are safe, effective and genuinely clinically useful.
Call to arms
Clinicians see the inefficiencies that are harming patients daily. Poor information transfer between primary and hospital care, non-adherence with treatment, and poor engagement with chronic disease care are examples in which the correct digital health intervention may reduce preventable patient morbidity and unnecessary health care costs.
Selecting the correct problem to address in health care is paramount and necessitates a clinician’s insight. Too often, digital health innovation has been focused on building the next “Uber for health care” or “10th-generation stethoscope”, building solutions without problems. The clinician’s insight is a valuable commodity in health innovation.
Our team of clinicians founded CancerAid when we saw that patient symptoms were often missed in oncology care, and that a mobile application could support the communication of symptoms between patient and clinician. Clinician involvement in health innovation allows us to shape the tools we use tomorrow.
Further, the clinician’s understanding of how new therapies may integrate into existing clinical systems is valuable. The real-world interaction between patient, clinician and therapy may be as influential in a patient’s health outcomes as the initial efficacy of a medication or procedure. From the outset, the development of a new digital health innovation should consider how it may integrate into existing workflows, and clinicians are well placed to provide input into these discussions.
Health innovation is an opportunity to make an impact on a broader scale. Digital health innovations in particular are advantaged in that they may be scalable and replicable across many patient groups, outside those we care for individually. Building a scalable health innovation gives clinicians the opportunity to improve health outcomes both personally, and a broader level.
Considerations
If you are interested in health innovation, we hope to outline a broad framework of considerations and actionable steps that may assist you.
Test your idea and understand the problem. The lean start-up methodology, often used as the basis of developing new innovations, is not dissimilar to the scientific method in that it calls for the rigorous testing of ideas and hypotheses. Understand the problem from all stakeholders’ perspectives, including patients, providers and payers. Our own understanding of a problem or solution is often restricted to the stakeholder perspective we hold – colloquially, we are all wearing blinkers. Seek feedback and listen.
Seek support. Australia has a growing innovation community that may provide invaluable assistance. Start-up accelerators and incubators are emerging around the country and provide structured support in progressing your idea further. More importantly, they may connect you to others with complementary skills and experiences, and access to valuable initial seed funding.
The Australian digital health community remains small, and a number of online communities (here, and here) exist to support and mentor new ideas. Organisations including the Health Informatics Society of Australia provide introductory courses in health informatics and organise regular conferences to meet peers within this community.
Learn the regulatory landscape. Digital health is regulated to safeguard the privacy and security of the sensitive data our patients share with us. Relevant Australian and international regulations include the Australian Privacy Principles (APP), the Health Records and Information Privacy Act 2002 (NSW), the Health Information Technology for Economic and Clinical Health (HITECH) Act 2009, and the Health Insurance Portability and Accountability Act of 1996 (HIPAA). Appropriate protections must be accounted for from the outset in the design and development of any digital health tool. The Australasian College of Health Informatics provides an informative list of resources to learn more.
Further, the provision of any medical advice or treatment must be carefully considered. For initial guidance, both the Therapeutic Goods Administration and the US Food and Drug Administration provide thorough advice about what software is considered as a medical device and which safeguards need to be in place.
Commercial and clinical validation. “Prescribable apps”, artificial intelligence technology and other digital health innovations are entering routine clinical care. Like any novel therapeutic, these innovations require evidence to substantiate their safety and efficacy. Examine the evidence for analogous tools or models of care and consider these in your own design. In the long term, consider how you may clinically validate and build evidence for your own work.
Clinical benefits including improved patient engagement, quality of life and even survival can translate to economic savings and commercial value. Commercialisation may be important for your innovation’s sustainability and will rely on the four “Ps” of commercialisation within our health systems: patients, providers, payers (insurers) and pharmaceutical companies.
Challenges
Australia has the fundamental building blocks for a leading health innovation ecosystem. Our hospitals, universities and health institutions deliver world-class outcomes. As healthcare continues its digital transformation, ongoing improvements in outcomes demand innovation, best led by clinicians working within our systems.
However, significant challenges exist in achieving this vision. The uptake of health care innovation in Australia requires behavioural and cultural change. We fall at risk of developing “innovation theatres” with poor real outcomes, if we do not develop a more mature culture within our healthcare systems that is capable of trialling and implementing new digital initiatives.
Lastly, we need to better support and engage our clinicians who are interested in innovation. We have great potential to drive improvements from within our systems. However, established pathways, particularly within vocational training, are circuitous or ill-defined to use this creativity. The establishment of organised programs to better support clinician innovation, including leadership pathway programs and training flexibility, will allow us to better harness these talents.
The digital transformation of health care has immense promise for delivering improved clinical and health economic outcomes. Clinicians are best placed to ensure that new innovations are safe, effective and genuinely useful. Our healthcare systems need to evolve to enable clinicians to be at the forefront of this change, and for new initiatives to succeed. If we are to be successful – the returns will be significant.
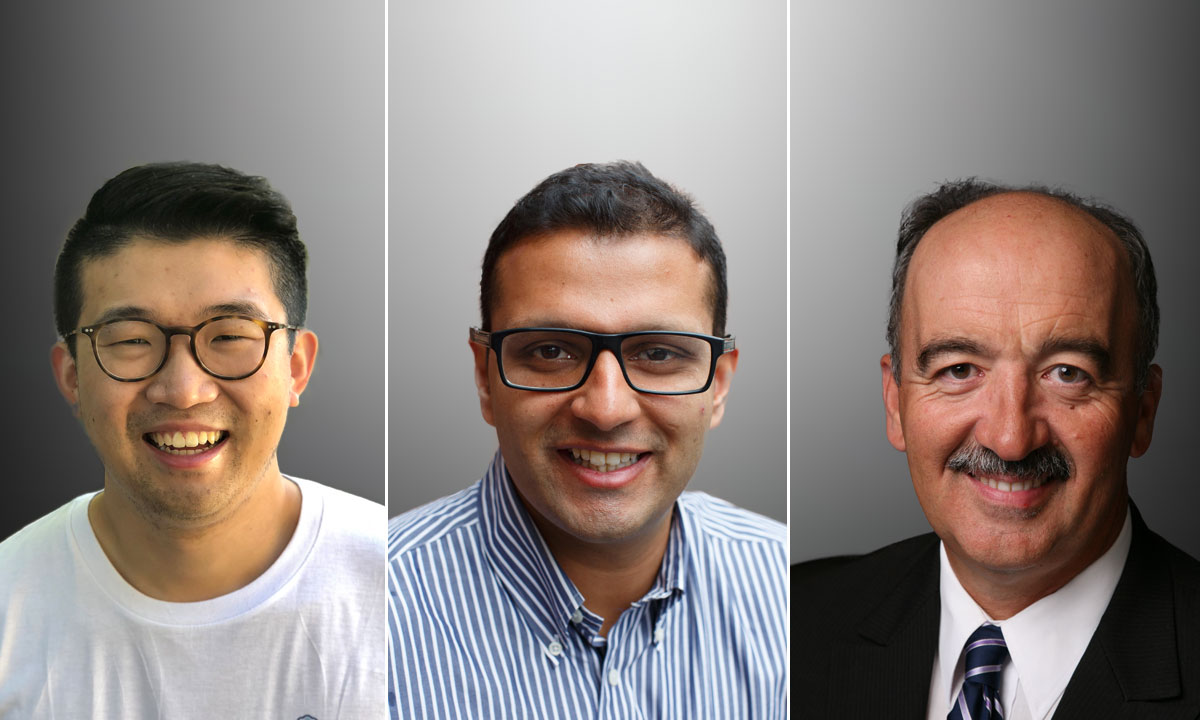
Dr Zachary Tan is a medical practitioner and a Director at CancerAid, a leading Australian health technology startup. Zachary is passionate about the intersection of clinical medicine, health systems and technology in improving healthcare outcomes on a broader scale.
Dr Raghav Murali-Ganesh is a radiation oncologist and the co-Founder and President of CancerAid. He has the ambition of improving healthcare outcomes with the use of digital tools.
Dr George Margelis is a medical practitioner who has been deeply involved in technology for the last 30 years. He was Chief Information Officer of a private hospital group as well as managing an innovative software development team. He is Adjunct Associate Professor at the University of Western Sydney with the TeleHealth Research and Innovation Laboratory and is also currently a member of Ignition Labs, a start-up incubator in the health space.
The statements or opinions expressed in this article reflect the views of the authors and do not represent the official policy of the AMA, the MJA or MJA InSight unless that is so stated.
To find a doctor, or a job, to use GP Desktop and Doctors Health, book and track your CPD, and buy textbooks and guidelines, visit doctorportal.

 more_vert
more_vert