TWENTY-two year-old Maria Lewis was at the gym, having just gone for a jog. Stepping off the treadmill, she felt a sudden blinding pain in her head. For a while, everything went white and she lost all vision. When her sight eventually came back, she had no idea what had happened to her.
“It was so intense, I’d never felt anything like it before, so I had nothing to compare it with.”
Thinking it may be a severe migraine, Maria got a cab home, swallowed some painkillers and took to her bed. But when she woke up a few hours later, the pain was still there and she wasn’t able to speak without slurring.
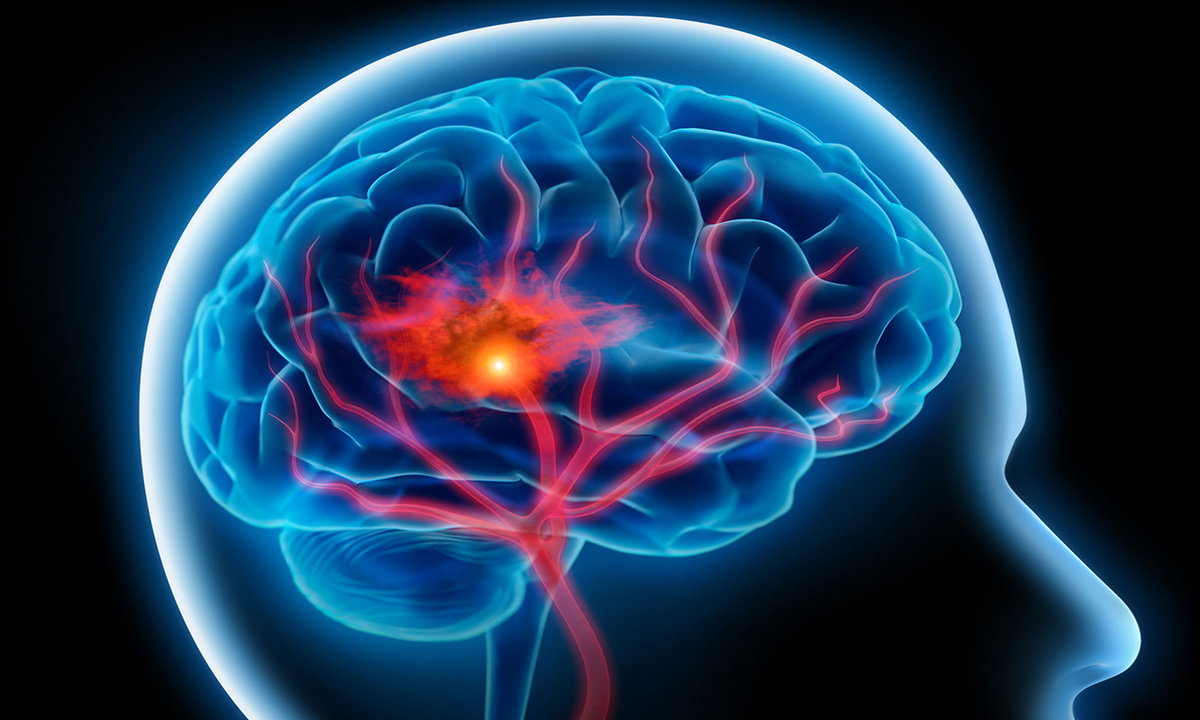
A friend drove her to the emergency room, where it took 24 hours for her to be diagnosed with transient ischaemic attack, or mini-stroke. Two weeks of in-hospital tests and rehabilitation followed, before Maria was finally discharged. She was back home, but her problems were far from over.
“For me the stroke was like an earthquake, and then for months afterwards, I continued to suffer the aftershocks and tremors,” Maria told MJA Insight. “But I was left too much on my own with it, and I didn’t know how to cope.”
According to a new Perspective published in the MJA, Maria’s experience is far from rare.
Its Queensland-based authors say that patients who had a minor stroke are not getting the care they need once they’re discharged from hospital.
“The problem is that these minor stroke patients, when they’re in hospital, look pretty good to their doctors, compared with the more acute cases,” said lead author Dr Emma Finch, a research fellow in speech pathology at the University of Queensland.
“They’re walking, they can have a conversation, and they’re in a hospital environment that is structured and supportive. But when they go back to their usual life, that’s when they run into difficulties.”
Dr Finch said that the problems these patients face can be quite subtle and hard to pick up in a hospital environment.
“It’s when they’re back home and they’re having to do family budgeting, or complex work-related tasks or participating in social activities that they may find these things much more taxing than before.”
Tenelle Hodson, a Brisbane-based occupational therapist who is working on a PhD in transitioning care for patients who had a mild stroke, said that executive functioning, attention and concentration, and organisation and planning were all areas where patients may experience ongoing difficulties that affect their daily life.
“Driving can be a big issue. Stroke patients can’t drive for a month at least, but when they return to driving, they may find that more complex situations, such as buses pulling out in front of them, or dealing with cyclists or oncoming traffic, are hard to handle.”
The MJA Perspective reports that around two-thirds of patients who had a mild stroke have difficulty returning to work, over a third of patients have reduced social activity up to 6 months after their stroke, and up to 29% report depression in the first year after the stroke.
With around 30% of mild strokes occurring in people of working age, these figures are particularly troubling.
But when patients encounter problems after discharge, they may find it hard to get the help they need.
“There are services, but it’s harder for mild stroke patients to access them,” said Dr Finch.
“We don’t have sufficient Medicare support. There’s a Chronic Disease Management program, but this gives Medicare rebates for only five sessions per calendar year. These patients potentially have a lot of different issues. They may have problems with speech, with balance or with depression, and five sessions across all the disciplines is not going to be enough.”
In Maria’s case, her problems included debilitating migraines every few months, and it took years before she found the right medication.
“I got depressed and there was a lot of anger, too. And there were memory lapses: I’d just forget things completely, what I called my ‘brain clouds’. My little trick is that I write down lists, which means I have a backup rather than getting mad at myself.”
And another problem, as a young woman, was contraception.
“Once you’ve had a stroke, they won’t let you go on the Pill, or any kind of contraception that involves the release of hormones, including implants and coils. That meant my only options were condoms or finding a doctor willing to fit me with an intrauterine device.”
But Maria, a journalist and author, eventually found some of the support she’d been craving through the Stroke Foundation.
“I was going through a difficult time and I found the Stroke Foundation website, where there’s a section called Stroke Stories. I found it endlessly helpful because reading the stories, I didn’t feel so alone anymore.”
Dr Finch said that communication was key to providing patients with the support they need.
“In hospital, patients should be told that they may experience various problems, which may be subtle but could compound over time. And they need to be told who to see when they encounter these difficulties.”
Ms Hodson said that a holistic approach was needed for the care of these patients, with GPs taking the critical monitoring role.
“It’s not just about secondary prevention but also about how people can adapt to changes in their lives, and talking to patients about these changes, because sometimes they won’t bring the issues up themselves.”
She said that health care providers can sometimes focus a bit too much on how the patient was functioning physically, rather than on their mental state.
“We’ve also got to look at how they’re going in everyday life, and refer them quickly on to the right people when problems arise.”
To find a doctor, or a job, to use GP Desktop and Doctors Health, book and track your CPD, and buy textbooks and guidelines, visit doctorportal.

 more_vert
more_vert