AN international study led by Monash University has found that nearly two in three women with polycystic ovary syndrome (PCOS) are dissatisfied with the length of time they wait and the number of health care professionals they have to see before receiving a diagnosis.
Women (aged 18 years and over) across 32 countries completed an online questionnaire, the results of which were “a damning report into our care”, according to Veryan McAllister, president of the Polycystic Ovary Syndrome Association of Australia.
Nearly half of the 1385 women surveyed in the study, which was published in the Journal of Clinical Endocrinology and Metabolism, saw three or more health care providers before they were diagnosed, and the diagnostic process took more than 2 years for a third of the survey respondents.
Professor Helena Teede, from Monash’s School of Public Health and Preventive Medicine and the lead author of the study, said that in addition, less than a quarter of the study participants were satisfied with the information they received from their doctors about common treatments for PCOS.
“Our findings show that women are dissatisfied with the diagnosis experience and that there are clear opportunities to improve awareness and health outcomes for women with PCOS,” Professor Teede said.
“The survey results will be used to inform international efforts to improve PCOS education.
“The real challenge is the lack of awareness about PCOS,” Professor Teede told MJA InSight.
“The Victorian Government has prioritised PCOS in its health plan, and the first statewide model of care will be starting in Victoria in February 2017, in response to the gaps in care [that exist].
“The model of care includes dieticians, psychologists, laser therapy, endocrinologists and an education program that will be codeveloped by health professionals and affected women,” Professor Teede said.
Ms McAllister said that the Monash-led study “verifies what we, the patients, have always known and experienced”.
“It is a damning report into our care; quality education, awareness and improved services are essential if we want to improve diagnosis and treatment outcomes for patients with PCOS,” she said.
“Between 9% and 18% of women of childbearing age have PCOS,” the authors of the study wrote. “Women who have the condition face an increased risk of developing diabetes, cardiovascular disease, and symptoms of anxiety and depression.”
“Given the high prevalence of PCOS, it is important for women and health care professionals to be more aware of the condition.”
“PCOS suffered from being badly named,” Professor Teede said.
“Despite the misleading name, PCOS is not primarily an ovarian condition, but instead a hormonal disturbance that is often inherited. PCOS’ diverse set of metabolic, reproductive and psychological features need to be addressed.”
PCOS is a chronic disorder that impacts metabolic psychological and reproductive health, especially infertility. Women are diagnosed with PCOS when they have at least two of the three key features of the condition:
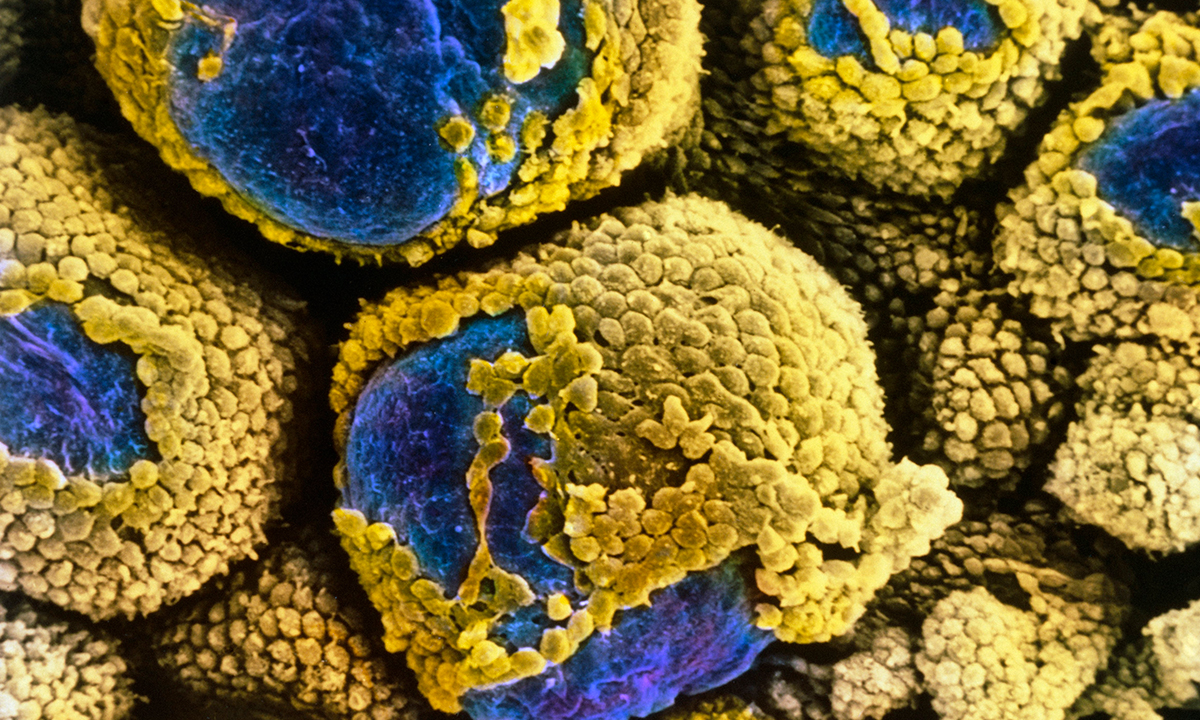
- ultrasound findings of immature eggs in the ovaries, which appear like cysts and are called polycystic ovaries;
- slightly higher levels of testosterone and other androgen hormones than average; and increased body and facial hair; and
- infrequent or no menstrual periods.
Professor Teede told MJA InSight that a set of international guidelines for the management of PCOS was being drafted by representatives from support groups from 22 countries and would be published some time in 2017.
Latest news from doctorportal:
- AMA, Govt hold talks on ‘more balanced’ approach to pathology rents
- Worrying MBS changes could be more than skin deep
- Blood clots more likely with testosterone
- Women don’t always get what they want from labiaplasty

 more_vert
more_vert