NEW funding enabling GPs to screen for diabetic retinopathy is a “victory for common sense” that will help eliminate needless blindness among people with diabetes, experts say.
As of 1 November 2016, GPs can use a non-mydriatic retinal camera to test for retinopathy in diabetic patients, rather than referring them to an optometrist or ophthalmologist for testing.
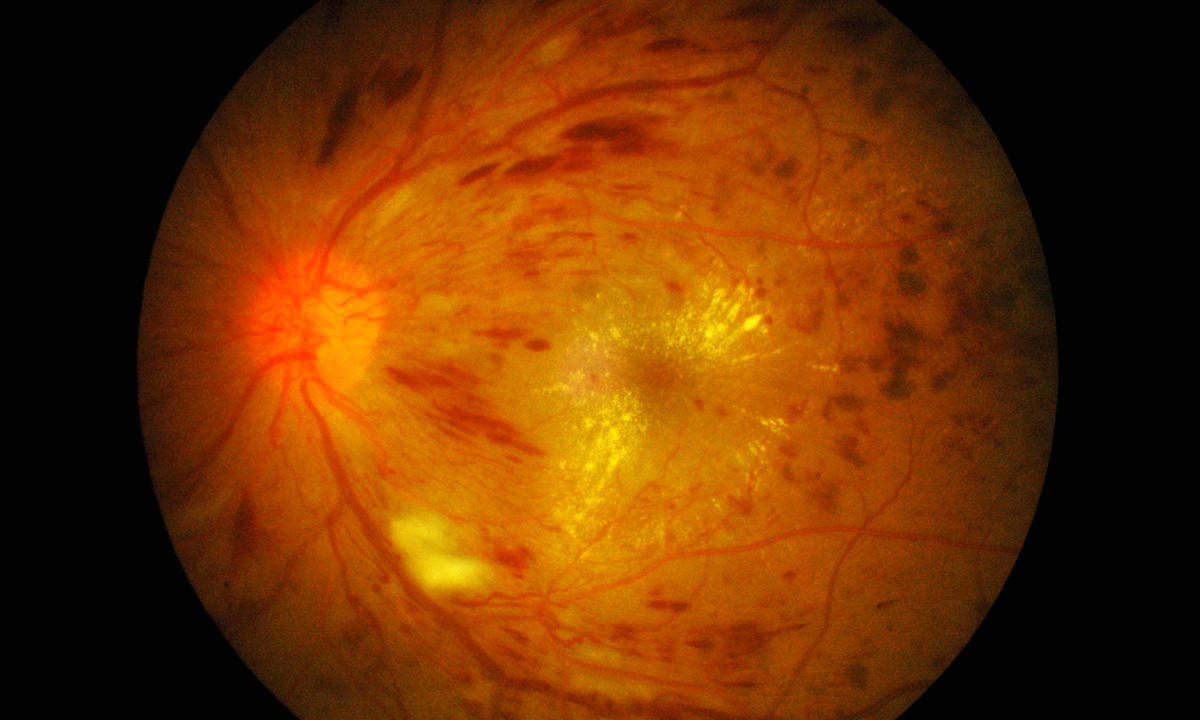
The new Medicare item numbers for non-Indigenous and Indigenous Australians, both with a schedule fee of $50, are expected to mean that fewer patients fall through the cracks by failing to present for their eye assessment. Currently, only 50% of non-Indigenous and 20% of Indigenous Australians with diabetes attend recommended eye examinations, even though the majority will develop retinopathy.
Laureate Professor Hugh Taylor, president of the International Council of Ophthalmology and the Harold Mitchell Chair of Indigenous Eye Health at the University of Melbourne, has campaigned for sustainable funding for screening retinopathy for over 2 decades and said it was a relief to see it a reality.
“People have been going needlessly blind for want of this service,” he told MJA InSight, noting that it was 2 years since the Medicines Services Advisory Committee approved the application.
“It has finally happened,” he said. “This measure is not only going to stop irreversible blindness, it will also save lives, because once you have gone blind it becomes very difficult to manage diabetes, to check blood sugar levels, to get to the doctor, to look at your feet and see ulceration, let alone do home dialysis.
“The presence of eye disease is a red flag for microvascular diseases in other organ systems – another reason why it makes sense for GPs to do the testing,” he added.
Professor Taylor said that Australia lagged behind many other countries in providing sustainable funding for retinopathy screening. England, for instance, had “basically eliminated diabetes as a cause of vision loss” by screening, he said.
The federal Department of Health said that the measure was expected to benefit around 370 000 people, and that roughly a quarter of those would be Aboriginal and Torres Strait Islander people.
Professor Sarah Larkins, a GP and associate dean of research in the College of Medicine and Dentistry at James Cook University, told MJA InSight: “This listing is a victory for common sense and increasing access of rural and remote populations to services many city residents take for granted”.
“Non-mydriatic cameras, which do not require the use of dilating eye drops, have been used in a range of successful state-funded outreach services and in the Aboriginal community-controlled sector since the 1990s,” she noted.
“Non-mydriatic screening is safer and much more pleasant for staff and patients than mydriatic screening, and as technology has developed, the images are now of very good quality,” Professor Larkins said. “However, the absence of a Medicare Benefits Schedule item number has limited the feasibility of uptake.
“This new measure has a lot of potential to reduce diabetic eye diseases, a common cause of preventable visual loss in our community, assuming adequate referral pathways are in place to access follow-up if required,” she said.
A variety of easy-to-use non-mydriatic cameras are available, although there is disagreement over whether the cheapest models are reliable.
Professor Taylor said that the typical price for a decent camera was $16 000 to $20 000. He recommended steering clear of cheaper mobile phone apps and attachments, which start at around $500, saying that “the quality and difficulty of use is against them all, as is the limited field of the photo”.
However, Professor Larkin said that some of the cheaper cameras may be sufficient for GPs, noting that many were available for around $5000.
“My personal opinion is to go for accessibility first and this means that the lower priced options are much more feasible for screening,” she said. “The higher priced units can be used by specialists to review those with an abnormal screening.”
The International Council of Ophthalmology offers a free online retinopathy grading course.
Latest news from doctorportal:
- Vaping ‘gateway’ to teen smoking: study
- Doctors ‘should report’ drivers with dementia
- Revalidation: what’s the problem?
- States to feel heat on doctor shopping

 more_vert
more_vert