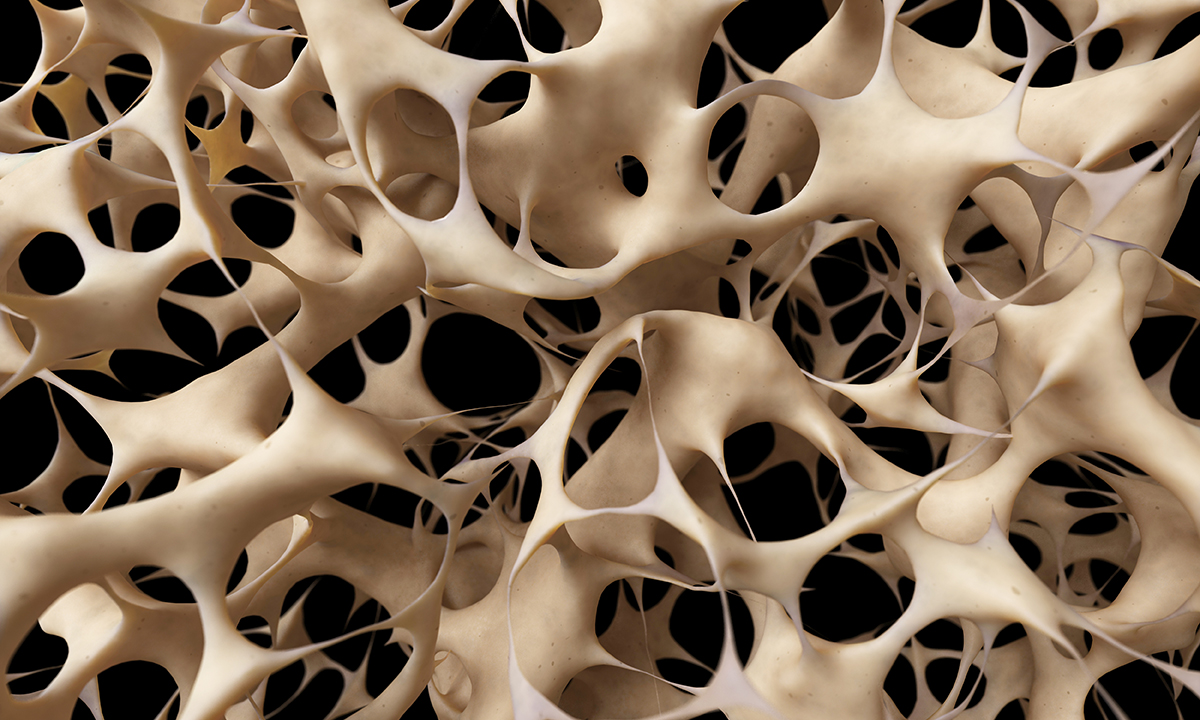
OSTEOPOROSIS is being under-treated across Australia, but integrated and evidence-based bone clinics are one solution to reduce the burden.
Professor Belinda Beck, a lecturer at Griffith University and director of the Bone Clinic in Brisbane, told MJA InSight that while setting up the clinic, which provides supervised exercise, dietary guidance and education, was a leap of faith, the decision had more than paid off.
“It had never been done before, but we knew there was a desperate need for it and the proof has been in the pudding.”
Professor Beck said that while medications could build bone and reduce fractures in some people, many others didn’t respond. Exercise, on the other hand, was an effective management approach – as long it was the right type of exercise.
“We have adopted a targeted evidence-based exercise program that is safe and effective for people at risk of fracture due to low bone mass when supervised closely in our facility.
“We think we have made the GPs job easier, because the Bone Clinic has a dual energy x-ray absorptiometry (DXA) scanner, exercise physiologist, dietitian and expert coaches all under one roof.”
Professor Beck was commenting on a narrative review published in the MJA which described osteoporosis treatment as a “missed opportunity”.
Osteoporosis currently affects 1.2 million Australians and, in 2012, fractures from osteoporosis and osteopenia in people aged over 50 years cost $2.75 billion.
The authors wrote that despite increasing therapeutic strategies for managing the condition, fewer than 20% of patients with a minimal trauma fracture were treated or investigated for osteoporosis, so under-treatment was extremely common.
“The time to close this gap between evidence and treatment is long overdue and will require systems-based approaches supported by both the federal and state governments.”
They wrote that one approach was fracture liaison services, which have proven to be cost-effective in reducing the burden of fractures caused by osteoporosis.
“General practitioners also need to take up the challenge imposed by osteoporosis and become the champions of change, working with the support of specialists and government to reduce the burden of fractures caused by osteoporosis in Australia.”
Adjunct Senior Lecturer Frances Milat from Monash University, a co-author of the review, told MJA InSight that given the increase in therapies now available for osteoporosis, treatments could be tailored to the patient’s age and comorbidities.
Adjunct Senior Lecturer Milat said that for GPs, there were excellent opportunities to consider osteoporosis management and assessment, especially in patients following minimal trauma, in men and women over the age of 70 years, and in patients treated with corticosteroids for more than 3 months.
“In these patients, Medicare rebates are available for bone mineral density assessment by DXA scan”, she said.
Tania Winzenberg, Professor of Chronic Disease Management at the University of Tasmania, told MJA InSight that as a common, chronic disease, osteoporosis was a “core business for GPs”.
“Nonetheless, as with all chronic disease prevention and management, prioritising and finding time for all the different needs of patients who frequently have more than one condition is a major challenge for GPs in managing osteoporosis.”
Associate Professor Morton Rawlin, spokesperson for the Royal Australian College of General Practitioners, told MJA InSight that osteoporosis has been an area of significant research and change since 2006.
“National guidelines are currently being revised and rewritten to reflect current evidence and best practice. It’s likely that continuing professional development will follow,” Associate Professor Rawlin said.
Professor Beck said that ultimately, the main thing Australia and the rest of the world were not doing adequately was preventing osteoporosis in the first place.
“For that to happen, it would require a quantum shift in the prioritisation of high intensity exercise introduced systematically from a very early age, coupled with an emphasis on a diet high in calcium.
“By the time a person is diagnosed with osteoporosis, normally in the later years, that horse has well and truly bolted.”
Professor Winzenberg said that if there was one change she could make to the health system it would be to ensure that all hospitals that treat acute fractures in older people have a secondary fracture prevention program integrated within them.
“This is a no-brainer of an intervention, with well established cost effectiveness, but one that is enormously challenging to implement with the current system of needing to convince every individual hospital to develop one.
“These services identify high-risk people, like those who have fractured, and ensure that they are followed up for appropriate investigations and treatment, and have a seamless transfer of care over to the GP,” Professor Winzenberg said.
Professor Beck said there were several reasons for the success of the Bone Clinic. First, people were able to feel a difference very quickly – they felt stronger, more confident and their quality of life improved.
“Equally, because most of our clients are older, another key to our success has been the atmosphere in the clinic. Nothing is scary, everyone is friendly and supportive and so it’s simply a pleasant and easy place to be.”
Latest news from doctorportal:
- Blocking overseas practitioners won’t solve rural doctor shortage
- AMA calls for independent scrutiny of asylum seeker health
- Medicines to treat side effects of other medicines? Sometimes less is more beneficial
- Hope for better kidney stone treatment

 more_vert
more_vert