THE world has just started to see the exciting potential of nanomedicine in the treatment of cancer, according to Australian experts, but several issues need to be addressed before the technology becomes more widely available.
Professor David Goldstein, senior staff specialist in the department of medical oncology at Prince of Wales Hospital, Sydney, told MJA InSight that Australia was actively involved in the global research effort into cancer nanomedicine, which “will ensure that we can get the right drugs into the patient, in the right place, at the right time, and with less side effects”.
As with any new medical treatment, determining which patients should get nanomedicine will be about weighing up the potential risks and benefits.
“This ratio has to be large. However, when patients have a malignancy, there usually is a relatively favourable benefit–risk ratio”, he said.
Professor Goldstein was commenting on an MJA editorial published online today, which described nanomedicine as “the technology of the 21st century” that would provide personalised, precision medicine tailored to an individual’s physiological make-up. (1)
Professor Zdenka Kuncic, of the School of Physics at the University of Sydney, wrote that in cancer nanomedicine, a wide range of nanoparticles were continuing to be developed for better tumour-targeted delivery of both chemo- and radiotherapeutics.
She wrote that these included liposome-, polymer- and micelle-based nanoparticles for encapsulated delivery, as well as metallic nanoparticles such as gold, which had been investigated for targeted radiotherapy.
Associate Professor Andrei Zvyagin, a biomedical researcher at Macquarie University, told MJA InSight that several nanoparticle formulations for the treatment of solid tumours were already commercially available.
He said the target mechanism of nanoparticles made these medicines very versatile and “especially effective for metabolically active, fast-growing cancers, such as several types of brain cancers and adenocarcinomas”.
In her MJA editorial, Professor Kuncic said that the single most important challenge for cancer nanomedicine was clinical translation and bringing the technology from bench to bedside.
The vast majority of the many different nanoplatforms developed for cancer therapy had not progressed past Phase II clinical trials, she wrote. Key difficulties included controlling nanoparticle size, preventing nanoparticle aggregation in vivo, biocompatibility and tumour cell specificity.
These challenges of clinical translation could also be viewed as opportunities, Professor Kuncic wrote. This was the approach taken by US National Cancer Institute’s (NCI) Alliance for Nanotechnology in Cancer. (2)
The alliance highlighted several opportunities for nanomedicine, including a stronger focus on developing active targeting strategies. It also emphasised the need for interdisciplinary collaboration in creating unique opportunities for breakthrough discoveries in cancer nanomedicine.
Professor Zvyagin said there were several other practical factors hampering the rapid uptake of nanomedicine cancer drugs.
“First, the cost of preclinical, clinical testing and other pharmaceutical certifications is very substantial — not only for nanomedicine, but for more conventional new drugs. It can reach several tens of millions of dollars, before these new drugs become available”, he said.
“The use of nanomedicine oftentimes also requires additional procedures to process a nanodrug immediately before its administration, along with concomitant equipment, staff training [and other resources]. Also, patient compliance is not always overwhelming.”
From the patient’s perspective, nanomedicine offered precision of treatment and a substantial reduction in side effects in normal tissue surrounding the tumour. However, the immune system could recognise these nanodrugs quickly, which could lead to deposits in the liver and other organs.
“This can induce toxicity. In order to evade the immune system response, contemporary research is addressing this problem [by] designing nanovehicles with controllable drug release”, Professor Zvyagin said.
Professor Stephen Leeder, emeritus professor of public health and community medicine at the University of Sydney and chair of the Western Sydney Local Health District Board, told MJA InSight that from a public health perspective, nanomedicine posed both economic and ethical questions.
“Like many of the new technologies, especially drugs, you can bet it will be expensive and products will be protected by patents. So ‘nanobots’ may be great for the rich but not available to the less affluent and the poor.”
Professor Leeder said this represented a general dilemma for those responsible for the wise allocation and spending of the health dollar, which “is not specific to nanotechnology but to all new interventions”.
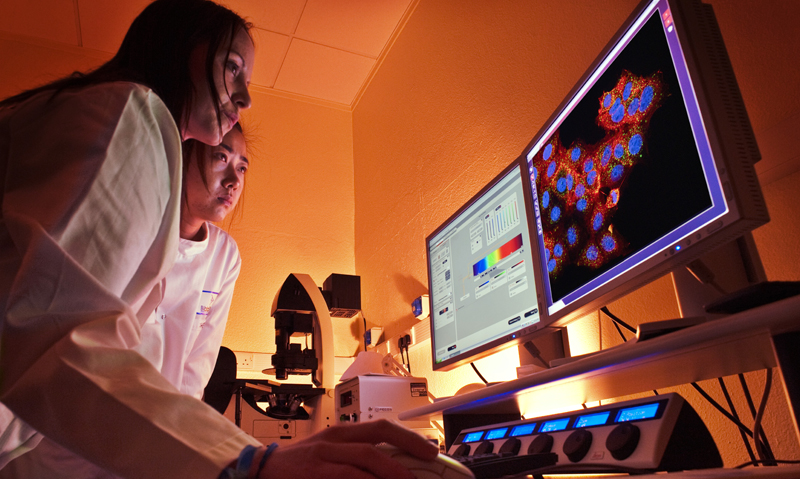
(Photo: James King-Holmes / Science Photo Library)
On MJA podcasts Professor Christophe Hagemeyer, head of the Vascular Biotechnology Laboratory at Baker IDI Heart and Diabetes Institute in Melbourne, discusses new nanotechnology which can deliver clot-busting drugs right to the clot.

 more_vert
more_vert