IMPLEMENTING the “exciting” advances being made in stroke treatment across Australia will be difficult without big changes to health infrastructure, training and resources, experts say.
Professor Stephen Davis, director of the department of neurology at The Royal Melbourne Hospital, told MJA InSight that the evolution of endovascular therapy represented “a huge paradigm shift in the management of acute stroke”.
“But this does mean that the health system must now be re-engineered to ensure patients have access to this treatment”, he said.
Professor Davis was commenting on an editorial published today in the MJA which discussed the “spectacular” results of recent neurointervention trials for acute stroke care. (1)
The trials all used either advanced imaging to identify patients who would respond well to reperfusion, or angiography to prove major vessel occlusion, or both, then randomly assigned these patients to receive endovascular reperfusion, usually in addition to alteplase thrombolysis, or standard acute stroke care.
The combination therapy resulted in potent reperfusion and a dramatic treatment effect, to the extent that three of the five neurointervention trials were stopped early, the editorial authors, Professor Richard Lindley and Professor Christopher Levi, wrote.
Dr Bruce Campbell, neurologist and chair of the National Stroke Foundation, told MJA InSight that from a physician’s perspective, endovascular therapy could be used in about 10% of all stroke cases.
“This may seem like a small amount, but these patients [with major vessel occlusion] are at the highest risk of death and disability from stroke.”
Dr Campbell led the Australian arm of a trial on endovascular therapy for ischaemic stroke, which found that when the therapy was initiated at a median of 210 minutes after the onset of stroke, it increased neurological improvement at 3 days. After 90 days, 71% of patients who had received endovascular therapy achieved functional independence, compared with 40% of those who had received alteplase-only treatment. (2)
The editorial authors said these trials highlighted that the “endovascular revolution” had arrived, and the health community needed to work quickly to redesign stroke care services and build a specialist workforce.
They suggested that a possible solution to the current shortage of neurointerventionalists was the emerging model to train neurologists in interventional neuroradiological skills, due to the growing consensus that a neurointerventionalist did not need to be a radiologist, provided they had received appropriate training.
In a written statement to MJA InSight, Professor Lindley, from the University of Sydney’s Westmead Clinical School, and Professor Levi, a senior staff specialist at the John Hunter Hospital, Newcastle, said that while the recent advances in neurointervention could make a dramatic difference to patient outcomes, their implementation in Australia will prove challenging.
“Interventional stroke management not only requires a high functioning stroke unit, but also the initial delivery of intravenous thrombolysis, and there remains a considerable gap between evidence and practice in the delivery of intravenous therapy.”
They said Australia also had a critical scarcity of expertise in the domain of endovascular clot retrieval, which represented the single biggest barrier to patients accessing these advances in stroke care.
Professor Graeme Hankey, professor of neurology at the University of WA’s school of medicine and pharmacology, agreed. He said it was important to drive the wider adoption of stroke treatment as a professional specialisation.
“Then we would have stroke specialists who are trained specifically in endovascular therapy”, he told MJA InSight, saying this would hopefully result in a more effective utilisation of hospital resources.
“This morning I saw three stroke patients, and several physicians were needed to treat each patient. But someday I hope that just one specialist will be needed to treat one incident of stroke”, Professor Hankey said.
However, Professor Davis said that while there was a lack of neurointerventionalists, it was important to guarantee physicians undertaking training in endovascular therapy were exposed to a large number of cases.
He said it would be preferable to have “a smaller number of specialised clinics with a very high case load, rather than having many centres being able to perform the therapy, but not very often”.
Dr Campbell said wide implementation of endovascular therapy in Australia posed a unique challenge.
“We are fortunate here in Victoria that we have both stroke and interventional teams working in specialised centres”, he said. “But Victoria has the advantage of a more compact geography — it is going to be hard to provide endovascular therapy in other parts of Australia.”
In Queensland, for example, most interventional expertise is located in Brisbane, but this is too far away for stroke patients living in Far North Queensland to access.
Professor Hankey warned that these issues must be addressed quickly as Australia’s growing and ageing population meant demand for stroke specialisation would only continue to rise.
(Photo: Arno Massee / Science Photo Library)

 more_vert
more_vert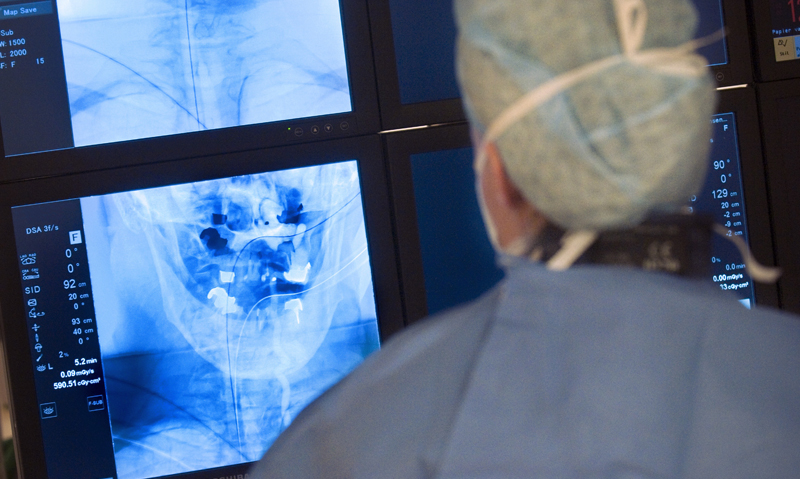
The main issue with the study described here is that it compared intravascular thrombolysis with systemic thrombolysis – when both therapies are controversial and neither can be considered a “gold standard”. The authors admit that the evidence for intra-vessel thrombolysis remains mixed, as is the systemic thrombolysis data. Only a small minority of stroke patients qualify for either treatment. It’s hardly time to reorganise the entire medical system around delivering either therapy. On the other hand, high quality post-stoke rehab therapy is applicable to all stroke patients and carries few if any risks. Why not put our money there?
Which gap between evidence and practice are the Professors referring to? The predominance of negative trials, trials stopped early due to clear harm (death) – juxtaposed to the highly editorialised reporting of a minority of trials showing any benefit (with statistical manipulations and post hoc analyses) from intravenous thrombolysis for acute stroke would point to thrombolysis being an unproven therapy (albeit with some potential, if we could continue to study the populations involved…)
The assertion that the success of endovascular removal of thrombus is contingent on initial thrombolysis is not supported by any study (that i’m aware of), as thrombolysis was required in both arms of the relevant studies of endovascular treatment. Indeed, it seems fanciful that both therapies wish to claim such amazing benefits in series – when it is much more likely that tight patient selection delivers the actual benefits seen with endovascular therapy to a small subset of all stroke patients. There is probably little benefit with IV thrombolysis, except in equally highly selected patients (but whose characteristics we still haven’t elucidated yet, due to the early cessation of our research into the matter…) The elements of current stroke care that aren’t as “exciting” as thrombolysis and clot retrieval are actually more supported by evidence, and can be delivered in most hospitals. We might have to concede that our allied health colleagues have more to offer our stroke patients, than does our medical expertise. A bitter pill to swallow, I know….
Re-engineering our stroke intervention infrastructure seems premature, until further pragmatic study is undertaken
Well if there was an Interventional Neuro-radiologist (or equivalent) on every street corner it would make no difference.
There are actually enough for now given the current level of infrastucture and organisation.
Some are underutilised, isolated, and/or performing other duties. So let us organise and support those who are currently in practice. Then high volume centres will be able to safely train the necessary additional workforce as needed. Ad hoc training as a knee jerk is not appropriate.
Mike