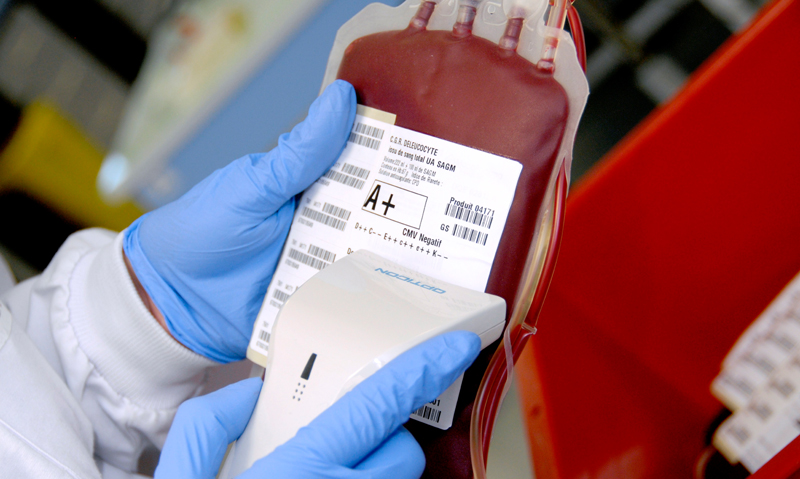
WORLD-first patient blood management guidelines developed in Australia have reduced demand for packed red blood cells by more than 16% and led to significant cost savings, according to the general manager of the National Blood Authority.
Leigh McJames told MJA InSight that the patient blood management (PBM) guidelines represented a landmark move away from the previously liberal approach to blood transfusion to a more restrictive and conservative process. (1)
However, Mr McJames said the shift has been driven by much more than cost-efficiency.
“There has been a shift in the belief systems in clinical practice. Blood transfusion is now viewed like a liquid organ transplant, where there are just as many risks to consider”.
Mr McJames was commenting on a US study published last week in JAMA Surgery which assessed the economic impact of liberal blood transfusions. (2)
The authors used data on haemoglobin (Hb) levels that triggered a transfusion as well as overall blood product use among 3027 patients who underwent pancreas, liver or colorectal surgery at a US hospital between 2010 and 2013.
Guidelines defined a liberal Hb trigger as the transfusion of packed red blood cells (PRBCs) for an intraoperative Hb level of 10 g/dL or greater, or a postoperative Hb level of 8 g/dL or greater.
The authors found that 942 patients received at least one PRBC transfusion — 8.7% during the operation, 14.2% during postoperative care and 8.2% during both. A total of 4000 units of PRBCs were transfused in the intraoperative and postoperative periods.
The results demonstrated that overuse of PRBC transfusion in surgical patients was common, the authors wrote. “More than 1 in 10 units of PRBCs were transfused using a liberal Hb trigger.”
By avoiding liberal PRBC transfusion, institutional transfusion costs might have been reduced by between US$27 360 (AUS$ 31 170) and US$94 516 (A$114 590) a year for patients undergoing these surgeries.
“Our data support the use of patient blood management systems to identify and reduce the liberal use of PRBC transfusions in the surgical patient”, the authors wrote.
Dr James Daly, haematologist and council member of the Australian and New Zealand Society of Blood Transfusion, told MJA InSight that “there is no doubt that blood transfusion is a lifesaving intervention that underpins much of modern healthcare, but there are also risks associated with transfusion”.
“Several prospective randomised studies have now compared liberal and restrictive transfusion thresholds in various clinical settings, and most have shown that clinical outcomes are not worse by restricting blood transfusion”, Dr Daly said.
Dr Axel Hofmann, visiting professor from the institute of anaesthesiology at the University Hospital of Zurich, told MJA InSight that the results of the JAMA Surgery study were directly applicable to the Australian context, where there “are even higher acquisition costs for blood components than in the US”.
Dr Hofmann co-authored an Australian retrospective cohort study of all multi-day acute care inpatients discharged from a hospital service in WA between 2011 and 2012. (3)
The mean inpatient cost was 1.83 times higher among patients who received a transfusion compared with those who did not. The authors estimated that the total hospital-associated cost of red blood cell transfusion in this study was $77 million, representing 7.8% of total hospital expenditure on acute care inpatients.
Mr McJames told MJA InSight the significant cost of blood transfusion, combined with the considerable risks to the patient, including sepsis, thrombosis and autoimmune reactions, underpinned the “precautionary principle” of the PBM guidelines.
The guidelines stress that blood transfusion should not be the default decision, and emphasise the need for careful consideration of how to help patients optimise and conserve their own blood.
Professor James Isbister, consultant haematologist in the Sydney Medical School at the University of Sydney, told MJA InSight the guidelines had helped make “blood transfusion a patient-focused process, not a product-focused one”.
Professor Isbister believed the implementation of the guidelines was assisted considerably by the “complete cooperation between the clinical community and the government”.
He said the states and territories had been developing their own PBM-based approaches, and a study recently demonstrated the effectiveness of the NSW Blood Watch program. (4)
The study showed a 27.4% reduction of blood usage after the introduction of the program, with reductions consistent across five elective surgical groups. The reduction was associated with annual cost saving of more than $8.5 million.
However, Dr Daly emphasised that ensuring the appropriate use of blood products was only one aspect of making the blood sector as efficient as possible.
“Transfusion laboratories and hospitals are also looking at the amount of blood they hold and how they can reduce the number of units that expire before being transfused.”
1. Patient Blood Management Guidelines
2. JAMA Surgery 2015; Online 6 May
3. Transfusion 2014; Online 8 December
4. Vox Sanguinis 2015; 108: 393–402
(Photo: AJ Photo / Science Photo Library)

 more_vert
more_vert