AUSTRALIAN research reveals “worrying” variability in mortality rates after heart valve surgery depending on the surgeon’s volume of experience with the procedure, but experts say super-specialisation is only part of the solution.
The study, published in Heart, Lung and Circulation, found risk-adjusted mortality rates 30 days after a valve operation ranged from 0% to 17% when comparing different hospital–surgeon combinations. (1)
Surgeons who had performed more valve procedures had lower 30-day mortality and complication rates compared with those with less experience. However, only valve-specific experience, not cardiac surgery experience in general, was linked with better outcomes.
Outcomes were found to be more uniform after coronary artery bypass graft (CABG), with mortality rates ranging from 0% to 1.6% with different hospital–surgeon combinations, with no significant association between volume and outcomes.
The study authors said their findings supported the case for subspecialisation of surgeons specifically within the field of valve surgery, saying this “may well result in lower mortality and morbidity rates”.
However, they warned of several challenges, including that “further specialisation may impair the skill of the surgeon in managing emergency or salvage operations in areas external to their subspecialty”.
The study included 145 surgeon–hospital combinations for isolated CABG operations and 122 surgeon–hospital combinations for valve surgery from 2001 to 2010, and was based on data from the Australian and New Zealand Society of Cardiac and Thoracic Surgeons registry.
Professor Paul Bannon, the society’s president, agreed that the variability in valve surgery mortality rates was “concerning”. However, he said it might have been driven by process factors such as the absence of multidisciplinary teams to ensure appropriate patient selection.
“Surgeon volume is often used as a crude surrogate for competency but it doesn’t tell the full story”, he said.
“We need subspecialists to perform these kinds of highly complex procedures, but even more crucially, we need multidisciplinary teams and supportive environments for the younger and lower volume surgeons”, Professor Bannon said.
In such an environment, surgeons and units could “have low volume and still get good results”.
Professor Bannon said the more uniform mortality rates with CABG in the study reflected that CABG was a fairly “uniform procedure, with clear guidelines”, compared with valve surgery.
Valve surgery involved a more heterogeneous patient group not always amenable to accurate risk calculations, he said. For instance, mortality risk in valve procedures was substantially affected by pulmonary hypertension, mitral annular calcification and whether the operation was post-infarction.
Professor Guy Maddern, head of the discipline of surgery at the University of Adelaide and clinical director of the Australian and New Zealand Audits of Surgical Mortality, agreed the wide range in mortality rates after valve surgery was “worrying”, saying some surgeons and units may need to increase throughput and reconsider patient selection.
However, he stressed that “better outcomes may not necessarily be because the surgeon has done a better job, but because the complications are better managed in high-volume settings where they have intensive care and radiology departments who are used to doing the rescue work”.
It made sense to concentrate the most complex surgery into tertiary centres to improve outcomes, Professor Maddern argued. He gave an example from WA, where the postoperative mortality rate for pancreaticoduodenectomy fell from 16% to 0% between 2010 and 2012 after the state government required the procedure be performed only at teaching hospitals with appropriate personnel and multidisciplinary support. (2)
Despite concerns from rural residents about being unable to access complex surgery outside of the major centres, Professor Maddern said “the inconvenience is worth it because you’re saving a life”.
Other procedures where a relationship between surgical volume and outcomes had been demonstrated were abdominal aortic aneurysm repair, oesophagectomy and liver resections, he said.
1. Heart Lung Circ 2014; Online 4 December
2. MJA 2013; 199: 539-542
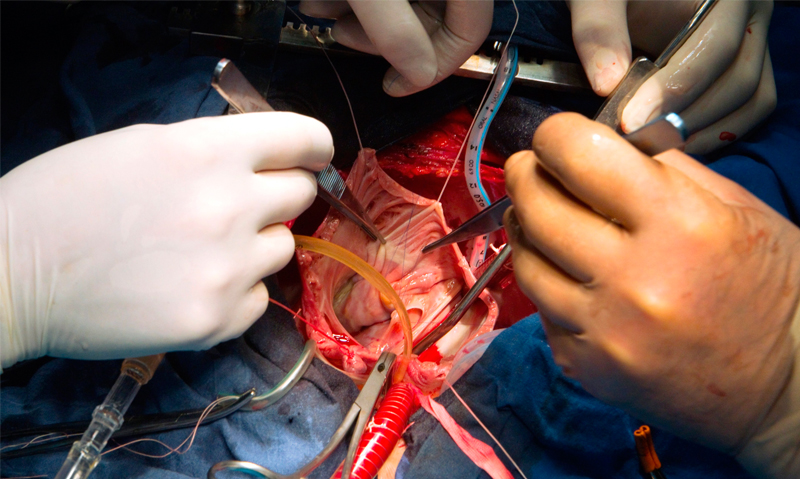
(Photo: Ria Novosti / Science Photo Library)

 more_vert
more_vert