LEADING neurologists have condemned an Australasian College for Emergency Medicine decision to fund its own analysis of thrombolysis for acute stroke, which the college claims would be free of the conflicts of interest that plague existing guidance on the treatment.
The Australasian College for Emergency Medicine (ACEM) is inviting proposals for consultants to analyse the published literature on thrombolysis in acute ischaemic stroke, which it has refused to endorse as a standard of care. (1)
Professor Yusuf Nagree, chair of the ACEM Scientific Committee, said unlike reviews published to date, its analysis would be “uniquely independent”.
“We are trying to find researchers who have no preconceived views or biases”, he told MJA InSight. An expert advisory panel would also be established to support the project, including an emergency physician, neurologist, GP, public health expert and lay person.
A Cochrane review published earlier this year found thrombolytic therapy significantly reduced death and dependency rates at 3‒6 months after stroke, and that this overall benefit was apparent despite an increase in symptomatic intracranial haemorrhage and deaths at 7‒10 days. (2)
However, Professor Nagree argued the review may have been undermined by conflicts of interest among its authors, who reported receiving payments from Boehringer Ingelheim, manufacturer of the recombinant tissue plasminogen activator alteplase.
He cited a review of the 20 most cited articles on stroke thrombolysis, which found 85% disclosed pharmaceutical sponsorship. (3)
Professor Nagree said there were several methodological flaws with the major trials to date, including the subjectivity of functional outcomes and selective allocation of patients to the intervention and placebo groups. “Of the 12 trials looking at the efficacy of thrombolysis for stroke to date, only two showed a benefit.”
He described the college’s current position on stroke thrombolysis as “very neutral”.
“We have said that it is a potentially beneficial intervention for acute ischaemic stroke, but because of conflicting evidence, it cannot be considered a standard of care”, he told MJA InSight.
“There are significant risks associated with thrombolysis, including intracranial haemorrhage and early death.”
He predicted the review would be published by mid 2015.
“If thrombolysis is shown to be effective we have got a big issue with rural hospitals where the therapy is not well established as it is in the cities”, Professor Nagree said. “But if the findings are negative, then our tertiary hospitals will have to relook at what they’re currently doing.”
However, leading neurologists have lambasted the project as a naive publicity stunt, raising concerns that it could lead to patients forgoing potentially life-saving therapy.
Professor Christopher Levi, stroke neurologist and director of Clinical Research and Translation, Hunter New England Local Health District, said that around the world thrombolysis was the guidelines-recommended therapy for acute ischaemic stroke in appropriately selected patients.
“There are hundreds of doctors behind these guidelines. To imply that these people are acting as part of a conspiracy and are tainted is the medical equivalent of the climate science sceptics”, Professor Levi told MJA InSight.
He said it would be virtually impossible for the college to conduct a review free of conflicts of interest. “If you don’t have a conflict you don’t have an interest — what matters is how those potential conflicts and interests are managed.
Professor Levi said some hospitals had introduced models of care that bypassed unsupportive emergency departments to ensure appropriate patients received thrombolysis for ischaemic stroke. “In some places, patients are seen directly from the ambulance by neurologists or stroke physicians now.”
He said neurologists and stroke physicians were well positioned to weigh up the risks and benefits of thrombolytic therapy as they dealt with patients both in the acute phase and in the long term, monitoring their recovery.
Professor Craig Anderson, professor of stroke medicine and clinical neuroscience medicine at The George Institute for Global Health in Sydney, said there was a “clear net benefit from thrombolysis in ischaemic stroke, dependent on the time and location of the clot in the brain and size of the ischaemic lesion”.
Professor Levi told MJA InSight that currently 5%‒7% of Australians who had an ischaemic stroke received thrombolysis, while among those who present to hospital within the critical 3.5-hour window, the rate was around 25%.
He said a realistic goal was for 20%‒25% of all ischaemic stroke patients to receive thrombolysis through enhancing the ambulance system’s capacity to respond quickly and through appropriate patient selection.
However, a major challenge was overcoming the entrenched opposition to stroke thrombolysis among some doctors, he said.
1. ACEM 2014; Request for Proposal: Review of stroke thrombolysis
2. Cochrane Database Syst Rev 2014; (7): CD000213; Online 29 July
3. West J Emerg Med 2011; 12: 435-441
(Photo: Zephyr / Science Photo Library)

 more_vert
more_vert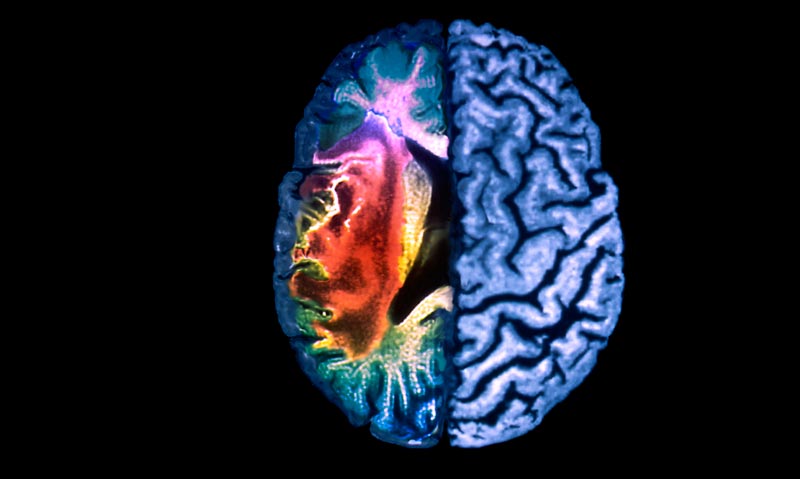
Andre makes a great point about being sued.
The problem is that the treating doctor on-site at the ED is liable , not leading Neurologists, nor the Physiotherapist co-ordinating the stroke unit,.
If any leading Neurologist was the only doctor at night in the rural ED, please tell us, would you treat a patient unconcsious with multiple injuries from an MVA, a febrile fitting child , a patient with a stroke, or a patient threatening suicide,, first? Which patient will you choose to transport first and last?
Even at Base Hospitals where there is CT scanning on-site, the scanner is not manned 24 hours per day, staff have to be called-in, and the reporting may be done remotely . delaying diagnosis .
Congratulations to the ACEM for funding analysis of evidence on treatment of ischaemic stroke.
Even if this does support thrombolysis, , who of the leading Neurologists will be available to work in rural hospitals where there is no FACEM, in person or by Teleconference, 24 hours per day, to accept responsibilty for thrombolysis ?
Would Prof Levi please enlighten us as to how the ambulances bypassing unsupportive EDs are diagnosing stroke , how they exclude TIA , atypical migraine, partial seizure, etc, and how many of these rapid-reponse stroke ambulances are operating in the Hunter New England Health service districts for how many stroke patients? Why is stroke more deserving of rapid-response ambulance than any other ED emergency presentation?
Equating thrombolysis sceptics with climate change deniers ( Prof Levi) . hmmmmm . That sort of statement worries me. What we don’t want is entrenched views that are not open to proper debate and question, because they have become part of a politically correct ‘groupthink’ in that area of specialty—- which is what has happened in climate science. Timely thrombolysis requires significant resources and changes to normal practice so we need to be sure it is worthwhile and with acceptable morbidities.
The idea that it is some sort of turf war is absurd. These are patients I am forced to deal with as we don’t even have a neurologist let alone a stroke physician. I am in a position where I am feeling pressured to give a treatment with questionable benefit and clearly has it’s risks repeatedly demonstrated. I am in a position where I could well be sued for not providing this so called ”standard of care”. This is happening in Australia.
I see my colleagues supporting this treatment despite their concerns about the lack of solid evidence because they feel pressured into doing so.
I would happily have someone take this out of my hands and take on the responsibility and risk although I do have concerns that patients are not being properly consented for this.
Without 24h interventional cardiology I frequently thrombolyse STEMIs whilst being cogniscant of the dangers. It doesn’t take too many intracerebral bleeds to give you a wariness of this drug.
I was berated by one of my best friends, a neurologist for ignoring “the overwhelming” evidence supporting thrombolysis yet he couldn’t even remember IST3. He went on to criticise emergency physicians in general saying they are not very good at diagnosing stroke. Such is the polarisation and emotion behind this issue.
We have a physiotherapist as our stroke coordinator pushing us to thrombolyse. She provided us with a survey asking us what would help us be more willing to thrombolyse. The options included a visit from an expert who would be the vocal Prof Levi. Well, the evidence is there for anyone to review. I wrote an alternate option, evidence clearly showing benefit.
I resent the term “turf war”. It implies that Emergency Physicians have something to gain by denying patients a potentially important therapy. We have been using thrombolysis in ED for 20 years – first for STEMI’s, now PE’s.Of course I want to give stroke patients in my ED the best possible chance, I just need to know that it really is providing more benefit than harm. We only have 2 large RCT for and 9 against, of course I’m uneasy and want more evidence. I’m sorry Etranger but the lead author of the Cochrane reviews has declared multiple financial ties to the manufacturer in the review. Apart from conflict of interest, the Cochrane review included 10 studies that were methodologically completely inappropriate (intra-arterial infusions, Chinese study with woeful methods, studies with n<50, nonclinical primary endpoints). It also had a high result heterogenity score (39%) which was ignored in the conclusion, and failed to account for the only other treatment – stroke units. Not all stroke patients make it to a stroke unit bed. I’m afraid the Cochrane review sucks, and I am delighted it is being redone in a completely above-board manner.
I agree with Ben regarding secondary prevention and rehabilitation.
Recently, one of my patients with Parkinsons’s disease had a fall, then a cerebral haemorrhage. He was transferred to the Base Hospital then tertiary centre-he was discharged, for “palliative care”., which the family understood meant he was going to die, soon, I insisted on Physiotherapy and active rehab. He is now walking, doing puzzles, and goes on pass with wis wife and sister and continues to improve.
While this is a case of cerebral haemorrhage, not ischaemic stroke, the role of active rehabiilitation applies to both. and in my opinion, is likely to be of more use in rural areas than thrombolysis, which is not achievable in rural areas due to demographis constraints..
The only data that is relevant is double blind randomised controlled trials and a very accessible way of getting a snapshot of these is on thennt.com. Registries and others are meaningless to the debate.
The drug company influence on this debate is very similar to the tactic used when activated protein C was pushed by publishing biased data and creating the surviving sepsis campaign. While the capaign has lived on, the drug has not.
There is no beneift to stroke thrombolysis and it sucks resources from more useful treatments and patients who need care and this is a huge under reported issue. The reason stroke outcomes have improved in recent years is the hard work of physicians providing secondary prevention, avoiding complications and rehabilitation.
If I cant verbalise my wishes when I come to an ED, do NOT administer thrombolytics to me for stroke. Even if I am 40 with 3 kids and am facing a nursing home drooling in front of them. At least then I might not die in the first 7 days (IST 3) and see their faces.
And thank heavens for an independent review.
[Comment modified: Editor]
Unlike the authors and respondents, i work in a rural/remote area where we cannot meet any of the criteria listed iin the article for stroke thrombolysis.
So please forgive my cynicism-the above article and responses have no relevance to where I work, nor to most of this decentalised continent.
Much of Australia is rural and does supply food to you urban experts, and a lot of coal and coal-seam gas to help the aircon and heating in your offices, not to mention the almighty export dollar.
Rural Australia struggles to staff rural health facilities with nurses or doctors, to treat the common presentations
So, I propose a study of how many patients at what cost in Australia have access to cerebral imaging within the window period of 3 to 5 hours after stroke, by demographic location-if it is zero in the area in which I work, then I apologise for my lack of interest.
Perhaps another study of efficacy of stroke prevention at what cost in Australia by demographic location could be done.
If stroke prevention is more efficacious and cheaper tghan throbolysis, , then I would suggest that emphasis on thomolysis in accute stroke is discriminatory., and should be described as best practice for the best located.
As to why neurologists are often in the “for” camp and EPs in the “against” camp is interesting. It’s not always the case -many stroke physicians railed against NINDS when it was first published, and a UK stroke physician appears to have driven the MHRA review- but you are right that it is the norm. I suspect opposing perspectives and conflicts of interest, leading to “different coloured glasses”, shall we say.
Stroke Physicians are faced with a disease that is difficult to treat- thrombolysis and mechanical interventions are probably their only treatments offerign any potential to reverse the disease. They are otherwise stuck with hoping for spontaneous recovery or a slow rehabilitation process. They are inclined to see a benefit that empowers them. Some also have financial conflicts, running huge units that receive a large income and kudos from thrombolysis, academic conflicts such that they need to defend their work, or financial ties with the manufacturer.
EPs are faced with huge demands, limited resources, bed-block and increased mortality from ED overcrowding. In this context we are told to facilitate an urgent treatment that sucks resources from a dysfunctional healthcare system, contributing to patients being deprived of proven interventions and diverting focus from more effective preventive health care. We have also seen many brave treatments for various acute conditions come and go. Therefore, before supporting major changes, many of us are inclined to be skeptical. The funny thing is that, unlike antivaxxers and climate change deniers, we don’t deny a potential benefit. We just want another trial to be sure.
As a member of the “small club”, I just happen to make acute thrombolsysis decisons one or twice a day, every day that I go to work
They weigh heavily on me, and I am gowing very tired of the fighting; often lead by people who don’t have to make those acute decisions and bear the consequences
I welcome the review, and look forward to it’s findings
Many times I have voiced my frustration at all this data rehashing, and emphasise that we should look forwards and develop better, safer and quicker treatments for stroke and ways to deliver them to as many people as possible
David Blacker
James Leyden you raise some interesting points, but in the end after years of internal discussion ACEM has taken the position to commission and independent review on behalf of fellows and the stroke patients we see in ED, and take as many steps as possible to exclude the vocal proponents on either side of the debate. Thrombolysis sceptics will have as much influence as thrombolysis zealots, zero. This approach has merit for the reasons I stated. Nothing to fear here and it has the potential to lower the temperature of the debate. Hopefully amongst he MJA readership ACEM receives many quality nominations to conduct the review or be part of the advisory panel.
There is no comparison with AVN, because we (unlike the AVN) are being quite logical and are not questioning “a huge body of Level 1 evidence”. Two things make good Level 1 evidence: (i) well-designed RCTs without evidence of allocation bias (inadvertent allocation of more seriously ill patients to one group) or measurement bias (eg open label studies), and (ii) replication (multiple RCTs), with more than one well-designed study.
Only one study of the <3 hour window (NINDS) has been positive, suffereing significant methodological issues as well as allocation bias. Their finding hasn’t been replicated, although the data as been re-analysed by two groups reaching opposite conclusions. Then there are two near-identical studies of the 3-4.5 hour window reached opposite conclusions (ATLANTIC and ECASS3).
The only “replication” has been pseudo-replication, i.e. registry studies. These have claimed a better outcome with earlier treatment. However, a more plausible explanation is that the studies include stroke mimics and TIAs(which have better outcomes), and that these are more likely to be treated earlier because they resolve quickly and will not be present in the cohort of patients treated later, which will consist almost entirely of established strokes.
The other argument is that meta-analysis solves all ills. It doesn’t because the meta-analysis is influenced by problems with the underlying data. Most disturbingly, recent meta-analyses have included IST-3, an open label study subject to major biases, and their claims of benefit have focussed on a subjective endpoint (functional status).
Its just a case of comparing the logic. I am not attacking anyone. Nor should any real argument descend into qualification comparison. Any group that argues against established evidence can be compared to the anti vaccination group can’t they – whoever they are? Isn’t that why we criticise them? There are similarities between anti vaccination groups ignoring the evidence and in this case ACEM by funding this. (Australian college of Emergency Medicine) . Just because an topic takes up space in a journal doesn’t mean its a valid argument! All journals – even the MJA love a bit of argument. Again this is where a climate change comparison is relevant. Still your case brings up the bias of which i speak: why is it always an ED physician arguing the antithrombolysis case and a stroke specialist arguing for thrombolysis? As for Bryan Walpole’s case – isn’t that comparable to the argument against vaccination by the mother of an autistic child? Surely case studies are not admissable in such a debate? Of course I know that plenty of ED physicians support thrombolysis, it just seems to be a particularly vocal powerful group within the ACEM running counter to evidence based medicine. Yes, a comparison to the dreaded AVN is revolting – but think about why that is. A group of people arguing against Level 1 evidence and using case studies to cause serious harm. Isn’t that exactly what the ACEM is doing by questioning the huge body of Level 1 Evidence here?
Jame Leyden- so there it is. In actual fact ACEM has no such bias. Some of its members have published in both camps and opinions are divided. ACEM is simply trying to work through the issue as best it can, and it is not alone. The BMJ recognises this as an issue requiring debate (http://www.bmj.com/content/347/bmj.f5215), and both the UK regulatory agency MHRA (Medicines and Healthcare products Regulatory Agency) and ACEP (American College of Emegrency Physicians) are also both now reviewing the issue in depth.
The telling thing here is the resorting to ad-hominem attacks such as comparison with anti-vaxxers and climate change skeptics.. what next? Let’s get back on track here. Emergency Physicians with MBBS, +6 yrs specialty training, +PhDs… these are the kinds of people raising safety concerns about thrombolysis for stroke.
The non-stroke physician equivelant to this announcement would be the Australian Vaccination Network asking for a review of whether vaccines cause autism, and claiming their “independent review” would be unbiased as opposed to the existing evidence. The College of Emergency physicians has a clear publication proven bias against thrombolysis – why should they be trusted? oh wait i forgot – the innocent have nothing to fear.
Etranger – your presumption was incorrect, I’m not referring to paying Neurologists to actually use thrombolytics, but to paying them to conduct research which supports an alternative use for a drug which is losing it’s original market (STEMI), and to spruik it at educational events. Not sure how my comment was misconstrued to suggest it was the Neurologists wanting independant research… they already have the “high moral ground” by controlling the meta-analyses!
Peter – great point re preventative care being a cheaper, less dangerous, and more effective approach. You also have to wonder when a group who would usually have the greatest natural inclination towards a quick fix for an acute problem (EPs) are unconvinced, perhaps the long-game approach has more merit.
Most, if not all emergency physicians want to give evidence based therapy, look at thrombolysis for AMI, antibiotic times in sepsis, and all those decision rules, for Radiology, pulmonary embolus. Evidence based.
Its just that with this particular therapy, the benefits are not so clear, and the downside is awful
I gave it to a 65 yo recently retired man with a hemiplegia, and he fitted then died in front of me, not evidence, but he would not have died from cerebral hemorrhage. He would most likely have lived without the drug I gave, on neurologists advice. We are all captives of our experience.
If the review is positive, we will all be happpier, and patients better. If negative, then I fear there will be more neurological trouble, as it is one of their few “effective” therpaies at present.
Etranger- I think there is a problem with the latest Cochrane review in that the authors may be conflicted by prior publication; it is generally best if Cochrane reviewers are not reviewing their own research. Why did they include a non-blinded trial (thus heavily biased) in the latest review, and why did they not highlight the underlying allocation biases of the only two suposedly positive studies? The data on which the review rests is thus heavily contaminated.
As to the turf war issue, perhaps. Interestingly we have had a few neurologists say to us privately “good job” when we highlight problems with thrombolysis but say “if I stand up and say the same thing, I will be ostracised/attacked by my colleagues.”
The neurology community is a small club and unfortunately, as suggested by Chris Levi’s comments in the interview above, perhaps suffering from “group-think comformity”. Conversely in the emergency medicine community we encourage open debate and scepticism, having seen too many “gold-plated treatments” come and go. Surveys indicate some emergency physicians think stroke thrombolysis works and many think it probably doesn’t work. Does this sound like a turf war or scientific medicine in action?
Conflict of interest and publication bias is a real issue and one that should be better adressed.
I’m an emergency physician that happens to agree that thrombolysis has net benefit in selected patients, especially in the sub three hour window. There are a number of my colleagues that disagree. One wonders what possible reason Dr Levi could have for opposing this review. If he is as confident of the evidence as he says, it is likely that an independent review will strengthen his position in this debate – enabling advocates for thrombolysis such as he and I to point out that the ACEM’s own review conducted free of industry influence found a net benefit.
Of note, the person or team selected on tender to conduct this review, and the expert advisory panel, with also have no record of publication or commentary EITHER for OR against thrombolysis. They will thus be as free as possible from influence by industry or entrenched position. Unless he fears the results, Dr Levi should drop his anti-scientific hyperbole and welcome this independent review.
RM – most of those 85% probably received funding for research from a pharmacetical company (BI or others), not to ‘support’ their product, by which presumably you actually mean pay to use? Not quite the same thing, is it?
You also miss the point that it ISN’T the neurologists who want new ‘independent’ research, it’s the Emergency Physicians.
This isn’t my area, (I’m not a neurologist) but it sounds a lot like another turf war is brewing……
Peter, that’s all fairly reasonable but it does ignore the fact that a lot of people will experience strokes until those preventative health strategies bear fruit in 20 years or so….
AH – there is already Level I evidence available (Cochrane Meta-analysis). By all means re-do the analysis but it won’t be any performed to any higher standard, unless you know of a better methodology! A properly conducted meta-analysis incorporates two elements, an assessment of methodological quality of the included (and, just as importantly, excluded) studies and an assessment of the outcomes, including adverse events. Without both of those, and an explicit examination of potential biases, then it’s not a meta-analysis.
The outcomes of another meta-analysis will only change should there be either (a) valid studies that were missed in the Cochrane review (unlikely, given the strict methodology employed by the Cochrane Collaboration), or (b) new studies published since the date of the review (possible, but generally a conflicting result will be shouted from the roof tops). The latter is the major reason why meta-analyses are periodically repeated.
Unless of course you feel that the Cochrane Collaboration is itself biased…..
And are we heading towards another “gold standard of care” that is determined by sub speciality neurologists and can only be delivered at great expense in a tertiary (or private) hospital with all the necessary expensive infrastructure?
What about the poor, the disadvantaged, the unemployed, the rural population, the Aboriginal population, the low literacy groups, the underserviced suburbs of the big cities?
Surely now more than ever, our research money and efforts should be going towards primary health/disease prevention strategies? Greater efforts in reducing obesity, smoking, Type 2 diabetes, hypertension etc will surely produce a far greater effect by reducing the causes of stroke – and be a more responsible use of country’s increasingly stretched health budget.
If, as seems likely, the next crop of trials demonstrate safe patient selection requires rapid access to specific imaging interpretation e.g. Diffusion /perfusion MRI, this will be another obstacle for implementation in remote areas. Telemedicine can help for the clinical assesment. I suppose if you dont want to do something you announce a review.
“If you don’t have a conflict you don’t have an interest”… I hope he was misquoted, as I’m sure it makes more sense to say “If you don’t have an interest you don’t have a conflict”. The laws of logic don’t allow you to have it both ways.
So why do Boehringer and other companies feel the need to pay 85% of published Neurologists to support their product? And why do those Neurologists now feel the need to obstruct an independant assessment of the safety of that product?
In the real world (outside trials) corners are being cut to fit patients into inclusion criteria, and at least at my hospital the Neurologists won’t release their local outcome data to demonstrate it achieves the outcomes seen in trials. J Hurley’s concerns are very justified.
I am self declared sceptic (Hurley JC. (2008) Tissue plasminogen activator for acute ischaemic stroke. Med. J. Aust. 2008; 188 (8): 488.) in regard to the limitations of the published studies for this particular therapy. However, the more important issue in my mind is safety. A key component of this therapy is accurate patient selection. Any benefit could easily be lost with poor patient selection.
If this turns out to be a good, clean review I don’t understand what the neurologists are angry about? Science is science. Numbers (when studies are conducted well) don’t lie. What’s the problems with getting more evidence out there?