 WE love paper. Just think about it — we use paper hospital notes, send each other printed or even handwritten letters, use paper radiology and lab forms, write or print our scripts, and we worship the voluminous textbooks on our shelves.
WE love paper. Just think about it — we use paper hospital notes, send each other printed or even handwritten letters, use paper radiology and lab forms, write or print our scripts, and we worship the voluminous textbooks on our shelves.
The good old fax machine, introduced in the 1970s, was much more successful in winning over health care professionals than e-health has been.
At the same time we feel the paper-dominated health care ecosphere is not very efficient, to say the least.
Many of us own a smartphone, tablet device or laptop and we love it. We make our devices sync with work email and agendas or other software. We may have a few cool apps. And about one in 10 Australian doctors is even using social media to connect with patients and other health professionals.
But in our day-to-day work, many of us rely heavily on paper and the fax machine. How do we change this?
In an innovative blog post titled “We have to wean doctors off paper. But how?”, a group of Silicon Valley designers explained how to make software for doctors more user-friendly.
To successfully design clinical software that competes with pen and paper, the authors mention three key factors — ease of use, flexibility and simplicity.
“If an [electronic health record] isn’t easy to adopt, doctors will quickly get frustrated and return to familiar paper. If it isn’t flexible, it will be impractical for many specialties and doctors with unique workflows”, the designers wrote.
In other words, medical software should be just as easy to use as paper.
Quick access to the clinical data is important. Long boot up times and multiple screens to click through should be avoided. Buttons and screens should be placed intuitively to reduce mouse movements and clicks.
But even if these three key factors are met, there’s still something missing.
Health care providers increasingly need immediate access to data. We’re connected 24/7 to networks and use so many different electronic applications to access all sorts of data sources, that it sometimes feels like it’s all too much.
How easy would it be if all the different tools were integrated in one software package?
The fourth requirement is integration of applications.
Imagine this: You’re sitting behind a large wide screen at work (see image below). If you click on the screen it responds immediately; the system is fast. The home screen provides online access to all the health providers in your direct network, including GP practices, specialists, hospitals, and allied health professionals at different locations.
 You can see who is online and who isn’t. Your incoming email and agenda sit in the right top corner, and in the bottom of the screen are your social networks of choice and a video consultation tool.
You can see who is online and who isn’t. Your incoming email and agenda sit in the right top corner, and in the bottom of the screen are your social networks of choice and a video consultation tool.
This mock-up screenshot is an example of the medical software of the future — a software package (in this case Best Practice) that integrates your favourite clinical software with Microsoft Outlook, a professional Twitter account, the practice or hospital Facebook page, Skype and Yammer. Users would be able to select their clinical or communication applications of choice (widgets) to appear on their personalised home screen.
Included in the package would be professional resources like electronic therapeutic guidelines, secure enterprise social networks and encrypted video consultation tools. Smartphone and tablet apps would be available to improve ease of access.
With two clicks of the mouse you can select and upload data from your clinical management software to the secure health network. Other health professionals can immediately read and comment on problems and questions. You can have a videoconference with colleagues while the patient data is still visible on the same screen.
Uploading or downloading personally controlled electronic health record (PCEHR) data is a matter of selecting the required data components and hitting a button. You can add or remove applications and change the home screen layout to suit your needs and (sub) specialty.
Medical software should be smoothly connected to cloud-based networks and be able to integrate desktop and mobile applications used by doctors in their day-to-day work.
With ease of use, flexibility and simplicity this will increase the uptake of electronic media by doctors — and help us forget our love of paper.
Dr Edwin Kruys is a GP at The Panaceum Group in Geraldton, WA.
2 October 2012

 more_vert
more_vert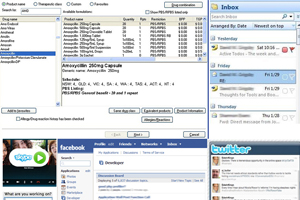
Although I have run a computer dealership since 1993, used computerised billing in my medical practice since 1987, and kept all my clinical records by computer since 2002, I am reluctant to embrace on line records for patient data or my own history. Put simply, I don’t trust any government controlled, or licensed, organisation to keep their servers secure from external hackers or corrupt staff. I think I am not alone.
Apologies for this delayed response (I was not aware of the comments on this site). I agree with longjohnsilver that digital solutions in the health care sector still have a long way to go. Many countries struggle with the same problem by the way. As Sue outlines, sometimes it’s easier to grab a piece of paper as it does exactly what you want! Still, I’m hopeful. We’re slowly moving into the eHealth direction. I feel we need more input from health practitioners and less IT consultants and eHealth ‘liaison offers’ at eg Medicare Locals. We’re the ones using it so we should take control and let developers and sponsors know what we need. That’s easier said than done, I know. I wrote a blog post about the 3 reasons why the PCEHR could fail (http://www.panaceum.com.au/pcehr/). Nevertheless, I’m an optimist and I use my blog to let the world know what doctors need to look after their patients properly. Let’s hope the world, and in particular policy makers, are interested in what health care professionals have to say. To answer your question Sue, I’m not aware that such a program exists but my experience is mainly limited to general practice. As we speak we’re working hard to optimise the software in our practices with about 70 users. It works, but is by no means perfect.
Thanks Edwin. I am a frequent and enthusiastic user of information and communication technology, where it HELPS me to function. In my working life, which relies on performing multiple tasks and having rapid patient turnover, the communication technology that I am provided with HINDERS my performance, and takes my time away from patient care. While the requirements of the digital system include individual log-ins, multiple page changes and electronic signatures at every step, the fastest way for me to record findings or order tests is still hand-writing on paper. If a system were devised that were not just paper-less but also faster and easier than writing on paper, I would go for it without hesitation. Do you know of any such systems that work in high-pressured rapid-turnover institutional environments?
Thankyou Edwin for your comments. The poll did not allow for a practice which is deliberately paper based and has no intention of doing otherwise unless much more user friendly by other means, no reliance on sites like the untrustworthy and un-professional facebook site or twitter and not dependant on such an unprofessional and unreliable file controlled by a manipulative patient. Many patients would not want their psychological or psychiatric profile open to all and sundry. Would you?
There is a long way to go before electronic records should be universal and mandatory. Queensland Health can’t even get the payroll right yet.