CLINICIANS need to be aware of changing patterns of infectious diseases, says an infectious diseases expert who has reported the first locally acquired case of a tick-borne infection.
“Infectious diseases never stay static”, Professor Peter Collignon, an infectious diseases physician from Canberra Hospital, told MJA InSight.
“I think clinicians need to be aware and concerned because as conditions change, so can the diseases”, he said.
Writing in the latest MJA, Professor Collignon and coauthors described the first case of human babesiosis thought to have been acquired within Australia. (1)
The 56-year-old male patient was found to be infected with Babesia microti — an organism never before detected in Australia.
The researchers were unable to pinpoint how the patient acquired the tick-borne infection as the only overseas travel he reported was a trip to New Zealand almost 40 years earlier.
“Its discovery as the cause of infection in this patient, who had no significant history of travel, raises intriguing questions about its natural hosts and epidemiology on this continent”, the researchers wrote.
They ruled out the possibility that the infection was caused by blood transfusion products or injecting drug use.
The patient, who lived on the NSW south coast, died from the infection in April 2011 after spending several months in hospital and despite treatment with recommended therapy.
Another article in the MJA also reflected the changing picture of infectious diseases. It described a recent huge spike in cases of melioidosis, in the Northern Territory’s Top End. (2)
In 2009‒2010, an unprecedented 91 cases of melioidosis were reported in the Top End, up from a median of just 27 cases annually in the 20 years to 2009.
The incidence of 50.2 cases per 100 000 in 2009‒2010 was the highest ever recorded in the melioidosis-endemic region of South-East Asia and northern Australia. The incidence among Indigenous Australians was almost twice as high at 102.4 cases per 100 000.
Researchers said the intense rainfall in the Darwin area at the time was considered the major contributor to the increase.
Among Indigenous patients, most cases in 2009‒2010 were reported in urban areas, a significant reversal from previous years where most patients were from remote communities.
A social change may have contributed on this occasion as remote Indigenous communities in the NT became “dry” following government intervention.
“… the Northern Territory Emergency Response initiated in 2007 may have had possible unintended consequences resulting from displacement of drinkers from remote communities to urban centres such as Darwin, where alcohol is available”, the researchers wrote.
Professor Collignon told MJA InSight the melioidosis research was a good example of how the epidemiology of well established diseases can alter due to a changing environment or population.
“Whatever we know today about infectious diseases will not be the case next year”, he said.
He said the research was relevant to clinicians Australia-wide, simply because people moved around.
“We’ve had people in Canberra [with melioidosis] who picked it up in the NT.”
Clinicians should ask patients about their travel history over the previous few years, especially if it was unclear why they were sick, he said. “Where people have lived and their travel history is really important. We see a lot of people with multiresistant bacteria after they’ve travelled to India or China.”
Another article in the same issue of the MJA found that Mycobacterium ulcerans infections were increasing in the coastal communities of the Bellarine Peninsula in Victoria. (3)
There was also a dramatic increase in activity related to Murray Valley Encephalitis activity, a mosquito-borne virus, across Australia in 2011, according to another article in the MJA. (4)
– Sophie McNamara
1. MJA 2012; 196: 350-352
2. MJA 2012; 196: 345-348
3. MJA 2012; 196: 341-344
4. MJA 2012; 196: 322-326
Posted 19 March 2012

 more_vert
more_vert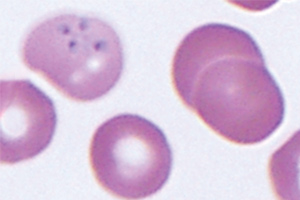
This story confirms what Australian doctors who treat tick-borne infections (including Lyme, Babesia, Bartonella and others), their patients and patient advocates have been saying for years. Health authorities and practitioners need to stay informed and open-minded about emerging infectious diseases. Instead, Doctors and patients have been unfairly marginalised for addressing these illnesses against the orthodoxy that “they aren’t here”. I look forward to more and better quality research about the prevalence and treatment of these infections in Australia and internationally.
Professor Collignon is spot on regarding the recognition of such diseases, including zoonoses, and has said what I have always suspected: that awareness of infectious diseases here by primary health providers, has been condensed to the Influenza group, the Hepatitis group, the AIDs group!
How about recognising that locally acquired Borellia infections (Lyme in all its flavours) is also present in Australia. It’s time authorities stopped putting their heads in dark places and looked at the records fron RNSH and evaluated them with an open mind. Given the past unreliability of testing, the current highly reliable testing done in USA at patient’s own cost should be taken for what they are, valid records of infections contracted in Australia. As my late mother would say, “none so blind as them that will not see”.